Evaluating PROs in immune-mediated diseases

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/73b79819-21b4-4207-b853-3d50b655beb9/18-RHE-1293-Abelson-Hero-Image-650x450pxl_jpg)
18-RHE-1293-Abelson-Hero-Image-650x450pxl
There is growing recognition of the value of measuring patient-reported outcomes (PROs) in patients with rheumatologic conditions. Clinical disease activity measures are important for making treatment decisions but sometimes do not measure the domains of health important to patients. PROs measured at point of care can enhance shared decision-making and facilitate treatment decisions, although the ability to collect and report PROs in real time can be challenging because of technology and workflow barriers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Through support from Cleveland Clinic and an information technology team, the Department of Rheumatic and Immunologic Diseases developed a patient-entered data (PED) system using validated measurements that assess physical and mental function, social health and well-being, and disease activity, as well as a rheumatology-oriented review of systems. This PED system, called MyRheum, allows the clinician to evaluate patient-reported health measures at point of care, engage patients in their care and make better treatment decisions based on patient-centric data.
At the 2018 American College of Rheumatology’s Annual Meeting, several staff members presented compelling data on their recent experience with MyRheum.
In “Using Patient Reported Outcomes at Point of Care in Immune Mediated Diseases: Minimal Clinically Important Differences,” authors M. Elaine Husni, MD, MPH; Chad Deal, MD; Abby Abelson, MD; Leonard Calabrese, DO; database designer Greg Strnad; and biostatistician James Bena shared how MyRheum helped evaluate PROs in several immune-mediated diseases.
Minimal clinically important differences (MCID) are patient-derived scores that reflect changes in clinical care that are meaningful to the patient. Little is known about MCID in many immune-mediated diseases, as small differences in PROs may be statistically significant yet clinically unimportant for the patient.
Using MyRheum, data was collected from patients with rheumatoid arthritis (RA), psoriatic arthritis (PsA), lupus and granulomatosis with polyangiitis (GPA) who had completed PROMIS GH and RAPID3 at two separate visits, six months apart. Paired t-tests assessed the changes between visits. Important differences were identified by a PROMIS MCID change of 5 and RAPID3-weighted score of 1.2 (improvement or worsening).
Advertisement
The authors found:
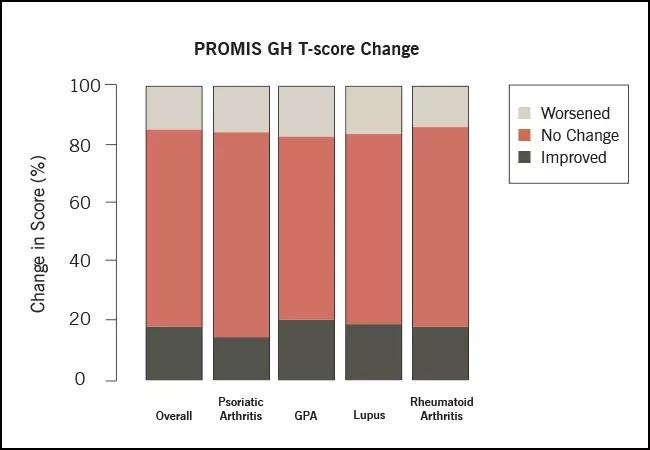
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d0cfba46-f301-424c-87a9-cc2584f29793/18-RHE-1293-Abelson-Figure-03-650x450pxl_jpg)
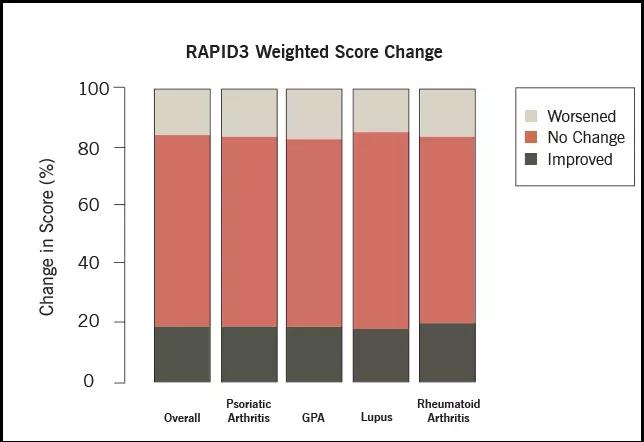
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4d8558ea-3730-4b0b-a2ca-cd2c1cedeb00/18-RHE-1293-Abelson-Figure-04-650x450pxl_jpg)
On average, there was improvement in PROMIS and RAPID3 scores among all immune-mediated diseases after two visits. However, this study indicates that it is unlikely to have a single MCID value applicable across all chronic diseases.
The variability in MCID implies that some patients improve while others worsen. This study presents an opportunity to better understand patient characteristics and therapies that may explain these changes.
Advertisement
Advertisement
Researching the biological basis for why treatment is or is not effective
Scribing system helps create more face-to-face interactions
A conversation with Leonard Calabrese, DO
The case for continued vigilance, counseling and antivirals
High fevers, diffuse rashes pointed to an unexpected diagnosis
No-cost learning and CME credit are part of this webcast series
Summit broadens understanding of new therapies and disease management
Program empowers users with PsA to take charge of their mental well being