Distinguishing the cause of fevers in patients with lupus

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3c5f9595-b567-4f3f-8356-ce1cca1f3239/18-RHE-1128-Littlejohn-Hero-Image-650x450pxl_jpg)
18-RHE-1128 Littlejohn Hero Image 650x450pxl
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 25-year-old female with systemic lupus erythematosus (SLE) manifesting with class IV lupus nephritis, lupus cerebritis, antiphospholipid syndrome, hemolytic anemia, oral ulcers, alopecia and arthritis was recently evaluated in our clinic for follow-up. Current therapy included prednisone, hydroxychloroquine and rituximab intravenous infusions, with the last dose given two months prior to this visit. She presented after a complex hospitalization during which she was diagnosed with atypical hemolytic uremic syndrome and received eculizumab therapy.
At our visit the patient endorsed feeling chilled, with myalgia and gastrointestinal upset. Her vital signs revealed that she was tachycardic to 130 beats per minute with a temperature of 38.6°C (101.5°F). She was promptly admitted to the hospital where blood work revealed elevated sedimentation rate (ESR) and C-reactive protein (CRP), and leukopenia with stable hemoglobin and platelets.
Rheumatologic diseases and their treatments often put patients at increased risk of infections. This leaves us keenly aware and constantly inquiring about infectious signs and symptoms. Herein lies one of the most common dilemmas faced by rheumatologists: distinguishing the cause of fevers in patients with rheumatic diseases. This is particularly true in lupus, where fevers can be a common manifestation of a lupus flare.
Research that can provide physicians with tools to elucidate the cause of fevers in lupus patients is ongoing. SLE activity measures — such as anti-double-stranded DNA antibodies, complements and the complete blood count — can be helpful, although these measures do not always track or change with lupus activity and certainly can be abnormal in the setting of infection. CRP and ESR, both nonspecific markers of systemic inflammation, are potentially useful biomarkers in this frequently encountered clinical scenario.
Advertisement
Interestingly, where ESR elevations are strongly associated with disease exacerbations in SLE, CRP levels do not tend to correlate with markers of disease activity, such as anti-double-stranded DNA antibodies and complement levels. The blunted CRP response in SLE patients may be due to the effects of interferon-a, a molecule highly expressed in lupus patients, by inhibiting CRP promoter activity and CRP secretion in hepatocytes.
Since ESR rises both with lupus activity and infection, alone it is too nonspecific to distinguish between lupus flare and infection. CRP values of >6.0 mg/dl in SLE patients have been associated with infectious processes and higher CRP levels have been observed in SLE infection compared to SLE flare without infection. When CRP is elevated during a flare, flares of serositis (pleuritis, pericarditis, pneumonitis) and flares involving nephritis or myositis present with a significantly higher CRP than other types of SLE flares.
In an article recently published in Lupus, a medical record review of hospitalizations of SLE patients was performed to assess the usefulness of the ESR:CRP ratio in distinguishing infection from flare in lupus patients presenting with fever.
Eligible hospitalizations for this study were those in which patients presented with a temperature of >37.9°C (100.3°F) or with subjective fevers as a chief complaint upon admission. Collected at admission were clinical and laboratory data, including patient symptoms, the infectious workup (X-rays, blood cultures, urine cultures), basic labs (including complete blood count), ESR and CRP.
Advertisement
We found that ESR levels were similar in patients with flares and infections. CRP levels were significantly higher in infections compared to flares (Table). The ESR:CRP ratio was positively associated with flare, where each unit increase in the ESR:CRP ratio was associated with a 13 percent increase in the odds of fever etiology being attributed to SLE flare vs infection. The proportion of flares vs infections varied according to ratio of ESR:CRP (Table and Figure), with infections predominant for ratios of ≤2, and flares predominant for ratios of ≥15 (P = 0.000).
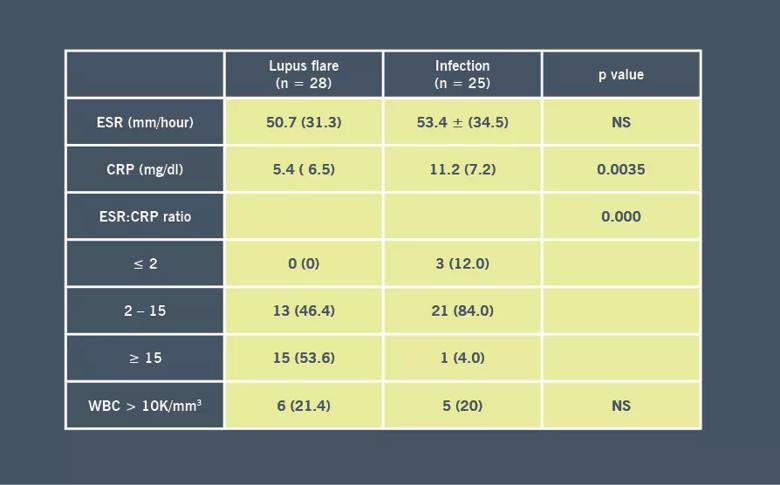
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d24bd2da-713a-41ab-a27f-b60ec462f694/18-RHE-1128-Littlejohn-CQD-Table-Inset-03_jpg)
Table. Non-specific markers of inflammation corresponding to episodes of flare vs infection.
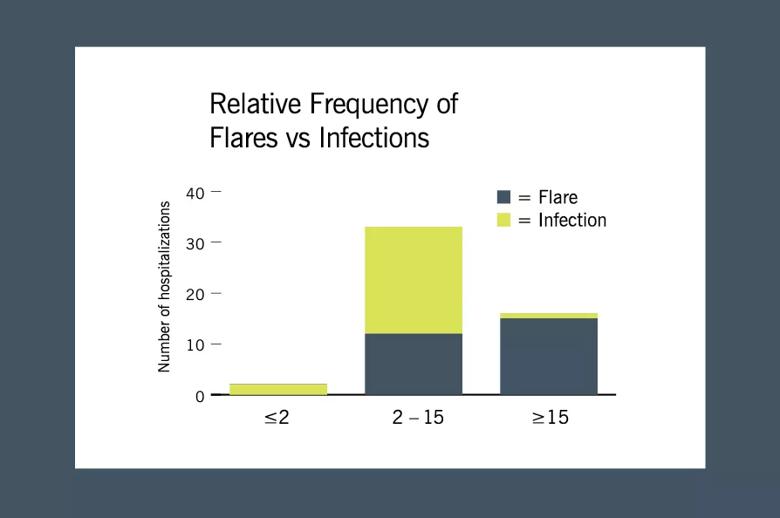
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6c358f87-c5eb-420d-9fc4-9dd642997a73/18-RHE-1128-LIttlejohn-Inset-02-Graph_03_jpg)
Figure. Relative frequency of flares vs infections according to erythrocyte sedimentation rate (ESR):C-reactive protein (CRP) ratio (categorized as ≤2, 2-15 or ≥15). There was a significant difference in the distribution of flares vs infections according to ESR:CRP ratio (P = 0.000).
Our patient was promptly admitted to the hospital where blood work revealed elevated ESR of 27 mm/hr (normal range 0-20 mm/hr) and CRP of 2.3 mg/dL (normal <0.9 mg/dL), with an ESR:CRP ratio of 11.7. Complements were normal, and anti-double-stranded DNA antibodies also were normal. Her complete blood count showed leukopenia, with both lymphopenia and neutropenia. Blood cultures grew methicillin-resistant Staphylococcus epidermidis, and our patient received a full course IV antibiotics, which resolved her fevers and normalized her cytopenias.
In summary, our patient was one with difficult-to-control, multi-organ-involved lupus; receiving ongoing immunosuppression; presenting with a temperature of 38.6°C (101.5°F). Blood work on admission was difficult to interpret, and there was a high suspicion of both infection and SLE flare. The ESR:CRP ratio was a useful tool in helping to guide the clinical acumen and delay use of high-dose glucocorticoids or other immunosuppressive SLE medications.
Advertisement
This precarious situation between treating an infection versus flare is not foreign to rheumatologists. In analyzing the usefulness of the ESR:CRP ratio, we hope to shed light on a potentially useful tool that can guide management in this common clinical conundrum.
Dr. Littlejohn is staff in the Department of Rheumatic and Immunologic Diseases.
Advertisement
Advertisement
Researching the biological basis for why treatment is or is not effective
Scribing system helps create more face-to-face interactions
A conversation with Leonard Calabrese, DO
The case for continued vigilance, counseling and antivirals
High fevers, diffuse rashes pointed to an unexpected diagnosis
No-cost learning and CME credit are part of this webcast series
Summit broadens understanding of new therapies and disease management
Program empowers users with PsA to take charge of their mental well being