Radiomic nomogram helps clinicians assess risk in patients treated with stereotactic body radiation therapy
Researchers at Cleveland Clinic’s Taussig Cancer Institute developed a risk calculator to predict overall survival of patients with non-small cell lung cancer (NSCLC) after stereotactic body radiation therapy (SBRT), and are sharing it publicly to help support clinical decisions. The research team demonstrated that use of the persistent homology (PHOM) score of a patient’s CT scan is the strongest predictor of overall survival of any standard clinical measure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Risk calculators are crucial for treating NSCLC, due to the high variability in survival rates. The team developed a radiomics nomogram as a new method of calculating risk beyond patient-specific histopathologic and clinical variables. Their work has been published in JCO Clinical Cancer Informatics.
“Traditionally, when we thought about patient survival, we relied on factors such as tumor size, patient age and whether the disease had metastasized,” says study co-author Jacob Scott, MD, DPhil. “Adding this radiomic nomogram to the mix transforms the way we predict outcomes. The best part is that this data is derivable from standard CT scans, and therefore it’s information we can have at our fingertips, without extra cost to the patient.”
A subdiscipline of machine learning, radiomics involves extracting high-dimensional data from images such as CT scans to better understand tumor biology and behavior. By extracting features from imaging data and applying predictive models, researchers can visualize disease characteristics not visible to the human eye. Previous radiomic scores were based on a standard set of measures, and were often not highly predictive in terms of patient prognosis. This measure, based on the radiomic quantification of solid tumor topology, is better able to gauge overall survival.
“We know that solid tumors have different geometric properties,” says lead study author Eashwar Somasundaram. “Benign tumors tend to be smooth while malignant tumors tend to be more diffused and ‘messy’, so the big question for us was: Could we quantify that ‘messiness’ to understand a patient’s overall prognosis? The answer is yes.”
Advertisement
Using a PHOM score, researchers can apply the mathematical technique of persistent homology to analyze and quantify a tumor’s structure so it can be used in predictive modeling. The researchers modified a persistent homology algorithm to accept CT scans. They then developed a method of taking a large matrix of data from each CT scan and synthesizing it into a single number. The resulting metric quantifies the 3D structure of a tumor and connect that to a patient’s clinical outcome.
“There were already existing PHOM algorithms for analyzing and condensing big data, but this approach preserves the overall structure of how data sets connect to each other, which is quite powerful,” explains Somasundaram.
In their original study, the researchers developed the PHOM score using CT scans from the Cancer Imaging Archive of 565 patients. In the follow-up study to create the nomogram, the researchers obtained CT scans for 554 patients with stage 1 or 2 NSCLC treated at Cleveland Clinic from 2008-2019. They calculated the PHOM score on each patient’s pre-treatment CT scan, combining it with clinical covariates to develop a prognostic nomogram.
PHOM score, age, sex, stage, KPS score, CCI and post-SBRT chemotherapy were predictors in the generated Cox proportional hazards models for overall and cancer-specific survival. Patients were split into high and low PHOM score groups by median value and compared using KM curves for overall survival and cumulative incidence curves for cause-specific death.
Advertisement
The PHOM score was a significant predictor for overall survival (HR: 1.17, 95% CI: 1.07-1.28), and was the only significant predictor for cancer-specific survival (1.31, 95% CI: 1.11-1.56) in the multivariable Cox model. The median survival for the low PHOM group was 45.41 months, which was significantly better than the high PHOM group at 29.18 months.
The score can also risk stratify within a given stage of NSCLC, so a patient with a low stage like 1a but a high PHOM score has a high risk of mortality. “This metric can stratify across all clinical groups, whether or not a patient has comorbidities, giving us a true measure of the tumor’s underlying biology,” says Somasundaram.
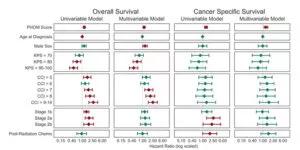
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/94a82816-4f95-4286-99a5-250cc94cf129/23-CNR-3647479-CQD-Inset-800x400-PHOM-score-300x150_jpg)
The PHOM score was the only significant covariate for both overall and cancer-specific survival. Bands represent 95% confidence intervals. The red bars represent significant hazard ratios.
In addition to helping predict overall survival, the risk calculator has the potential to guide clinicians in choosing the appropriate treatment option for each patient. “There is no trial comparing SBRT vs. surgery with definitive results, but this may support clinicians in determining what is the best treatment for any given patient,” says Dr. Scott.
This novel metric can be used along with other radiomic variables to aid clinical decision-making. The team is seeking research collaborations to expand on this work. To further validate the nomogram, they hope to study matched sets of patients with early-stage NSCLC treated with lung resection alone.
Advertisement
Advertisement

Treatment assigned FDA review date in June 2025

Cleveland Clinic, the University of Minnesota and University of Cambridge receive $1M grant to develop point-of-care biosensor for early detection and treatment personalization

Hybrid treatment model helps improve cancer care access
Resection, radiotherapy or ablation?

Extent of baseline burden impacts progression-free and overall survival

Quantum computing being studied as a means to help improve predictive performance, accuracy

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Targeting DNMT1 shows promise in chemotherapy- and immunotherapy-resistant SCLC