Alternative treatments for chronic pain are effective and available, but physicians don't always turn to them as first-line options
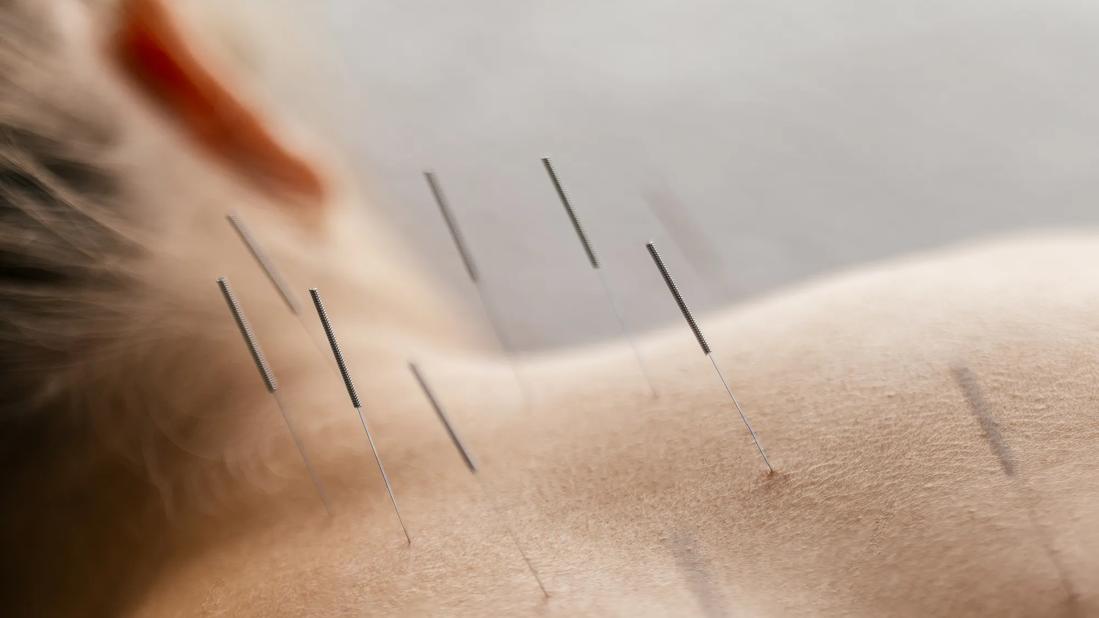
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/790c14b2-66ce-40ae-ad26-8f246c887b45/accupuncture-spine-1933009448)
Acupuncture
Chronic back and neck pain can be incredibly frustrating for patients looking for relief. When treating these patients, caregivers often turn to more aggressive treatments first while ignoring some of their noninvasive options. By first exploring more conservative options, such as lifestyle recommendations, acupuncture and osteopathic manipulations, they can provide patients relief without the need for pills, surgery, injections or other more invasive procedures.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When treating chronic pain patients, pain management and functionality are often the primary goal. “The vast majority of my patients increase their functioning as their level of pain decreases,” says William Welches, DO, PhD, a specialist in Cleveland Clinic’s Department of Pain Management. “They can handle pain, but what they can’t handle is the loss of function. I have one patient I treat so she can continue to run. She would have less pain if she didn’t run, but running is a big part of her life. I help to keep her functional in an activity that’s important to her.”
One of the simplest ways to improve functionality is through lifestyle modification. The Four Pillars Project — co-founded by Dr. Welches; and Teresa Dews, MD, President of Cleveland Clinic Euclid Hospital; and Robert Saper, MD, Head of the Department of Wellness and Preventive Medicine — is a new program that attempts to simplify and establish a base of treatment and education for pain patients. The program stresses the importance of sleep, stress management, appropriate diet and exercise.
“It turns out that the single best activity for us is walking,” explains Dr. Welches. “We’re designed to walk. I always recommend a 30-minute walk every day for every appropriate patient. It is the perfect activity for the kinds of problems, usually pelvic and spinal, that our patients come in with. If you’re walking naturally, it’s a very complicated process. You’re opening and closing joints in a very controlled fashion, and that is important in maintaining an aligned structure.”
Advertisement
Acupuncture is another tool that pain specialists can use. The origins of the therapy go back 4,000 years, and it can treat a wide range of patients and conditions. While Western attempts to explain how acupuncture works remain inadequate, clinical studies indicate that the therapy is effective at managing chronic pain.
“When we talk about acupuncture, we have to take off our Western cap and put on an Eastern cap,” says Dr. Welches. “That can be difficult for the patient, of course, but for the doctor too. Acupuncture requires a different way of thinking about a problem. One of the advantages of acupuncture, beyond the fact that it demonstratively works, is its broad range. A patient may ask me, ‘Will acupuncture help this?’ The answer is invariably yes.” Dr. Welches adds, “Oftentimes, I end up treating patients with both acupuncture and osteopathic manipulation because they’re complementary approaches. The effects can be synergistic.”
Osteopathic manipulation is yet another noninvasive treatment option. The primary goal for this type of treatment is to realign vertebrae in the spine to bring relief to patients with neck or back pain. “In my view, manipulation works best for mechanical pain,” explains Fredrick Wilson, DO. “We’ve got one vertebra sitting on top of another, and they’re all stacked down the line. Each one can be slightly out of its normal position and cause pain through localized muscle spasm. If I have someone with neck pain, I’ll go through their history and try to figure out if this is disk pain or mechanical pain or neuralgia. For example, if they’re complaining of pain with motion and it’s tender to touch, that sounds more like mechanical pain.” Dr. Wilson adds, “So what an osteopath does that an MD doesn’t do is we actually check the range of motion of each individual vertebra. If we find one that is not moving as it’s supposed to, that is called somatic dysfunction.”
Advertisement
There are two basic types of manipulation: direct and indirect. Direct manipulation takes a vertebra that may not want to go in a certain position and forces it to go that way. With an indirect technique, the osteopath actually takes the vertebra where it wants to go and holds it there, and the vertebra actually resets. Both Drs. Wilson and Welches use the indirect methods more often than some of the direct manipulations such as high-velocity, low-amplitude (HVLA) manipulations.
“I was never very comfortable with HVLA, which is where you get the so-called cracking,” explains Dr. Wilson. “So, I started using more of the soft techniques. For these techniques there’s one muscle energy and one counterstrain. If you turn off all the neurologic input coming in to this one spot, things quiet down and the muscles actually have a chance to just kind of relax again. In about 90 seconds, the pain is gone. You can literally feel it melt under your fingertips.”
One way to increase usage and acceptance of these noninvasive treatments is to reexamine the care path for chronic pain patients. Dr. Wilson teaches manipulation to Cleveland Clinic’s medical spine fellows, and he tries to help new specialists recognize these treatments as first-line options.
“A lot of our fellows are MDs, but some are DOs, so I feel like my job for the DOs is to reintroduce these techniques, because they’ve gotten away from them during an MD residency,” explains Dr. Wilson. “The MDs aren’t aware of some of these techniques; for example, I can feel a neck and recognize that this is off and this is off. MDs don’t think this way, so I help teach them that mindset.” He adds, “Every time they see someone with neck pain, I have them at least feel the area and ask themselves if this pain seems mechanical. If that’s the case, they can either learn these techniques themselves, or they can refer the patient to an osteopath who can provide them with these treatments.”
Advertisement
Advertisement
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology
Recommendations on identifying and managing neurodevelopmental and related challenges