Multi-institutional report indicates 100% success rate for treated patients
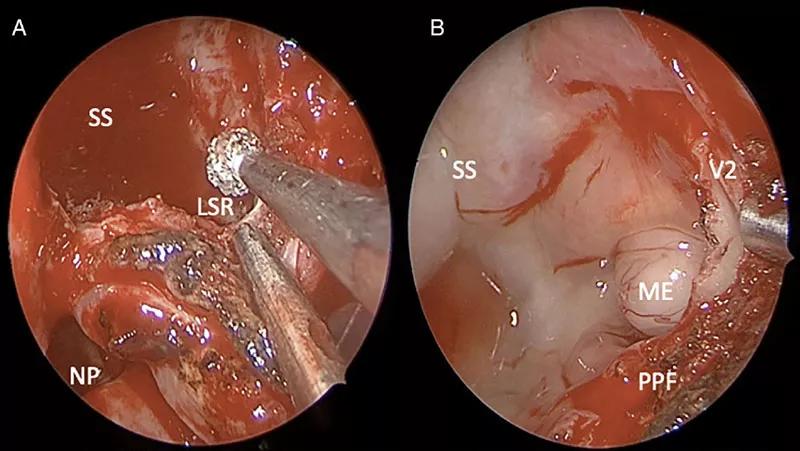
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a63ca344-e4f8-46f6-be30-ade6e36b9ebb/21-HNI-2270420-Lateral-sphenoid-sinus-surgery-tumors-CQD-fig3_650x450_jpg)
endoscopic modified transpterygoid approach (MTPA)
For meningoencephaloceles originating in the lateral recess of the sphenoid sinus, access can be extremely difficult. These lesions have traditionally been treated with invasive approaches including the transpterygoid or transmaxillary approach and even craniotomy. These approaches are associated with serious drawbacks including poor visualization and greater patient morbidity.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To overcome these shortcomings, skull base surgeons in Cleveland Clinic’s Head & Neck Institute have incorporated a different technique to treating patients with this rare condition. The simplified approach, referred to as the endoscopic modified transpterygoid approach (MTPA), allows the surgeon to access the lateral sphenoid sinus through the nasal cavity without having to dissect through (and possibly injure) the complex anatomy of the pterygopalatine fossa.
The original transpterygoid approach was described in 2005 and involved a technically challenging dissection of many important structures. “With the traditional approach, a surgeon has to go through the back wall of the maxillary sinus and through the pterygopalatine fossa in a straight line to get to the lateral sphenoid sinus,” explains Raj Sindwani, MD, Head of Rhinology, Sinus and Skull base Surgery in Cleveland Clinic’s Head & Neck Institute. “The problem is in getting there — you had to move sensitive nerves out of the way and avoid injuring them, dissect fat, manipulate lymph nodes and arteries, and then you finally arrived at where the problem is. The reason our modified technique would have been difficult to attempt back then, is that all of our instruments were straight and rigid, especially the tools we used to actually resect the meningoencephalocele and control bleeding. Now, some 15 years later, we operate around corners all the time using angled endoscopes and angled and malleable instrumentation. It was this angled instrumentation component that I think drove home to us that this approach was actually feasible and could offer significant advantages.”
Advertisement
Dr. Sindwani and his team have published two important studies detailing the success of this innovative approach. The first article, “Simplifying Access to the Lateral Sphenoid Recess: A Modification of the Transpterygoid Approach,” which was published in the American Journal of Rhinology and Allergy, describes the technical aspects of the endoscopic MTPA and why it should be considered for accessing benign lesions in this challenging location. The second article, published in Laryngoscope, and titled “Modified Transpterygoid Approach to Sphenoid Meningoencephaloceles: A Shorter Run for a Longer Slide,” reports a multi-institutional experience using this greatly simplified technique. One of the major findings from the second article is that of the 33 included patients treated with MTPA for meningoencephaloceles in the lateral sphenoid sinus, the authors had a 100% success rate and no recurrent cerebrospinal fluid leaks.
“By simplifying this otherwise very complicated technique, my hope is that we can help surgeons assist their patients by offering excellent outcomes and fewer complications.”
Cleveland Clinic performs this and other complex skull base surgery using a multi-disciplinary skull-base team approach, which includes a rhinologist and a neurosurgeon. Dr. Sindwani describes this approach as similar to a dance, where multiple instruments are going through the nose to remove the meningoencephalocele (or skull base tumor) and then patch the hole in the skull base.
“The patch can come from a number of different sites,” explains Dr. Sindwani. “In our experience, we’ve had such a high success rate with our technique, that we usually employ a small postage-stamp sized piece of nasal lining to patch the defect. Our results also demonstrate that by and large, more involved pedicled flaps, which we do sometimes use for more complex skull base reconstructions, are generally not needed for sphenoid meningoencephaloceles. Overall, between the simplified approach and the straight forward repair with free mucosal grafts, we are trying to advocate that when done well, less is more in these cases.”
Advertisement
While endoscopic MTPA has several benefits for the surgeon because of its less invasive approach and shorter dissection time, there are also a number of benefits for the patient. Most importantly, there should be far less risk of bad bleeding or injury to nerves which can cause temporary or even permanent dry eye, dry nose, and facial numbness. In addition, when a patient has this surgery, there are no cuts or bruises on their face because everything is done through the nasal passages. Dr. Sindwani also doesn’t use any nasal packing that has to be removed but instead uses just tissue glues and things that are completely absorbed away to support his repair. He notes that most of his patients are discharged home after just a few days, with follow-ups a week after the surgery and again around four to six weeks after that.
“Surgeons have been excited to hear that there is an easier way to get to the lateral sphenoid sinus and effectively manage these lesions without the complicated and risky dissection associated with older approaches,” Dr. Sindwani explains. “If you’re a patient, hearing of the excellent success rate and that this approach offers the promise of fewer complications and a better and a quicker recovery, that sounds pretty compelling,” he says.
Advertisement
Advertisement
Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor
Case study illustrates the potential of a dual-subspecialist approach
Evidence-based recommendations for balancing cancer control with quality of life
Study shows no negative impact for individuals with better contralateral ear performance
HNS device offers new solution for those struggling with CPAP
Patient with cerebral palsy undergoes life-saving tumor resection
Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition
Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.