Studies yield promising data in patients undergoing presurgical evaluation
Widespread use of MRI has revolutionized the diagnosis and surgical treatment of epilepsy, where identification of the underlying epileptic pathology is key. Even so, approximately 30 percent of patients who undergo evaluation for epilepsy surgery have a conventional MRI showing no abnormality. Management of this challenging group of patients requires further improvement of MRI’s sensitivity to subtle epileptic pathologies.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Progress toward such improvement has been on display at the 2018 annual meeting of the American Epilepsy Society, where a group of researchers led by Cleveland Clinic staff scientist Irene Wang, PhD, presented results from three recent MRI studies conducted at Cleveland Clinic Epilepsy Center. The studies highlight collective efforts by Dr. Wang and colleagues to translate novel MRI techniques to the everyday practice of epilepsy surgery.
The conventional MRI used for clinical purposes nowadays is an inherently qualitative imaging modality, with image intensity values varying significantly from scanner to scanner and from patient to patient. This partly explains why MRI lacks diagnostic specificity for the underlying pathology of neurological diseases.
MR fingerprinting (MRF) has emerged as an alternate imaging method that can successfully address problems associated with conventional and advanced imaging modalities, as outlined in Nature (2013;495:187-192) by researchers at Case Western Reserve University in Cleveland. MRF enables noninvasive quantification of multiple properties of tissue simultaneously through a novel approach to data acquisition, post-processing and visualization. The quantitative T1 and T2 measures generated from the MRF technique can be exquisitely sensitive to tissue alteration under pathological conditions.
Close collaboration among Dr. Wang and colleagues — Dan Ma, PhD, a Case Western Reserve research scientist and first author of the above Nature paper, and Stephen Jones, MD, PhD, a neuroradiologist in Cleveland Clinic’s Imaging Institute — led to intriguing pilot data showing that MRF has the potential to contribute to epileptic lesion characterization. Figure 1 shows 3D MRF images from a patient with right temporo-parietal epilepsy who had widespread epileptic lesions (periventricular nodular heterotopias). On a clinical MRI scan, the lesions appeared to have the same signal intensity. With MRF, a significant T1 increase in the MRF T1 map was identified at the right occipital horn nodules. This distinct signal abnormality was not appreciable on conventional MRI. Upon subsequent invasive evaluation with intracranial EEG, these nodules were confirmed to cause the patient’s epilepsy; surgical resection rendered the patient seizure-free through eight months of follow-up. These intriguing pilot data were presented at the AES meeting.
Advertisement
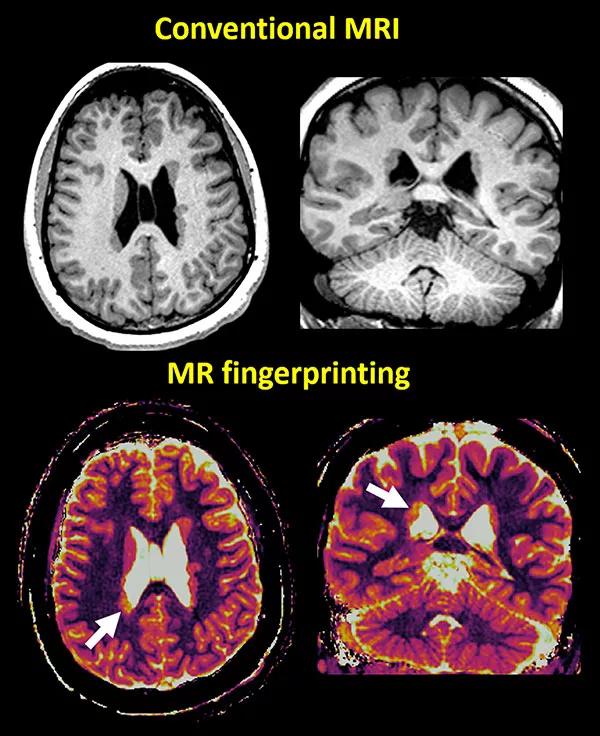
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/092f0d3a-9997-4e34-83a7-3e14c060a975/18-NEU-5853-MRIfingerprinting-inset1-600x736_jpg)
Figure 1. 3D volumetric MRF acquisition from a patient with periventricular nodular heterotopia. Top: T1-weighted MRIs from clinical scans in axial and coronal views. Bottom: T1 maps from the 3D MRF scan in axial and coronal views showing the nodules at the occipital horn of the right lateral ventricle (arrows) representing significantly higher T1 values, differentiating themselves from the other nodules. This information was not appreciable on the conventional clinical MRI. The nodules with the higher T1 values were later confirmed to have caused the epilepsy in this patient, who is now seizure-free after resection.
In addition to MRF data presented at the AES meeting, the first results on 15 patients undergoing epilepsy presurgical evaluation with MRF at Cleveland Clinic Epilepsy Center are being published in the Journal of Magnetic Resonance Imaging (in press). In four of the 15 included patients (who had varying types of epileptic lesions), MRF was able to show additional, clinically relevant information not revealed by conventional MRI. “These promising data suggest that researchers and clinicians may soon have a novel tool at hand to examine intrinsic properties of epileptic pathologies at a finer level than previously possible,” says Dr. Wang.
In an earlier study in Annals of Neurology (2015;77:1060-1075), Dr. Wang and colleagues reported that computer-assisted analyses of conventional clinical MRI, using a voxel-based morphometric post-processing method, can lead to an increase of up to 40 percent in the detection rate for patients with subtle epileptic pathology. Two additional studies presented by Cleveland Clinic researchers at the AES meeting further explore the usefulness of this technique in cohorts with challenging epilepsies arising from the cingulate cortex and the orbitofrontal cortex, respectively.
Advertisement
Study in cingulate epilepsy. Surgical management of patients with epilepsy from the cingulate cortex is highly challenging, especially in the setting of negative MRI. Due to this region’s deep location far from the brain surface, commonly used localization tools such as scalp EEG may be misleading or unhelpful. Seizure activities originating from the cingulate cortex also spread very fast. As a result of these challenges, intracranial EEG, an invasive procedure, is mandatory in almost all patients with suspected cingulate epilepsy.
In this retrospective analysis, nine patients with epilepsy from the cingulate cortex were studied. MRI post-processing detected structural abnormalities in six of the nine patients (example shown in top panel of Figure 2). All abnormalities detected by post-processing were concordant with ictal onset on intracranial EEG when such testing was performed. In the meantime, in the same cohort of patients, the localizing yields of noninvasive tests such as scalp EEG, PET, ictal SPECT and MEG were relatively limited. “These results suggest that MRI post-processing should be incorporated into routine surgical evaluation to enhance detection of subtle epileptogenic abnormalities in this especially challenging population,” observes Dr. Wang. The study was just published by Dr. Wang’s group in Frontiers of Neurology (2018 Nov 27 [Epub ahead of print]).
Study in orbitofrontal epilepsy. MRI post-processing similarly works on epilepsy coming from the orbitofrontal cortex, as demonstrated in a retrospective study of eight Cleveland Clinic patients with epilepsy arising from that site. Epilepsy from the orbitofrontal region is difficult to recognize and easy to misinterpret as either frontal lobe or temporal lobe epilepsy. Lesion or subtle changes in the orbitofrontal cortex are difficult to identify visually due to the region’s complex gyral and sulcal convolutions. With post-processing, the majority of patients in the study (seven of eight) showed a subtle abnormality in the orbitofrontal region (example shown in top panel of Figure 2). “Again, these new data suggest the necessity of adding this noninvasive test to the patient evaluation process, for the purpose of better guiding intracranial EEG implantation and resection,” Dr. Wang notes.
Advertisement
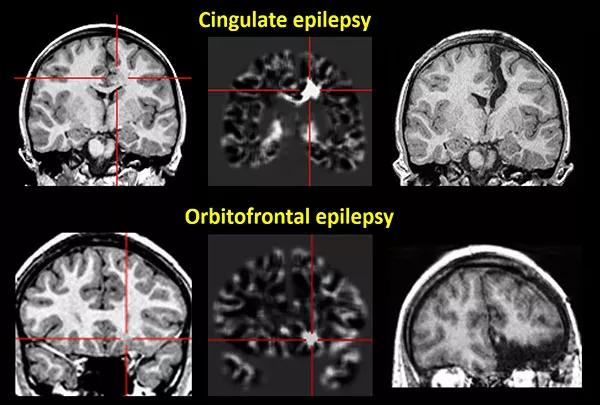
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/34a6fb0c-13e9-4386-878b-4ada43c772f3/18-NEU-5853-epilepsy-inset2-600x405_jpg)
Figure 2. Representative imaging from two patients in whom computer-assisted analyses of conventional clinical MRI pinpointed subtle epileptic abnormalities. Top: A patient with epilepsy from the left middle cingulate cortex. Bottom: A patient with epilepsy from the left orbitofrontal cortex. Left: Conventional MRI used for post-processing. Middle: Statistical maps generated from post-processing, highlighting the abnormality. Right: Postsurgical MRI showing complete resection of the lesions leading to sustained seizure freedom.
There is still a significant unmet need for MRI tools to rapidly, quantitatively and reliably measure pathologic substrates in epilepsy, Dr. Wang notes. “The next step our team will undertake is to combine the novel MRF techniques with post-processing analyses,” she says. “This promises to lead to the newest and most sophisticated neuroimaging techniques, ones that may have the ability to revolutionize epilepsy care.”
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help