Results may refine surgical selection criteria and advance clinical trial design
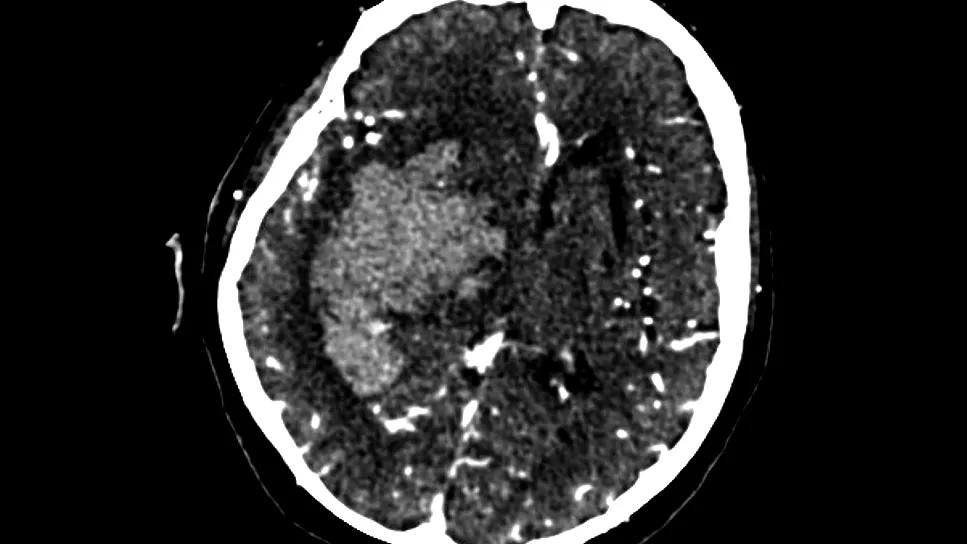
A computational morphological model of basal ganglia intracranial hemorrhage (ICH) based on preoperative CT angiography can serve as a prognostic tool to help determine candidacy for minimally invasive surgical evacuation. So suggests a new study that describes the model design and its potential utility compared with traditional prognostic tools used for patients with a basal ganglia ICH. The single-center Cleveland Clinic study was published in the Journal of Neurointerventional Surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our model of basal ganglia hemorrhage morphology predicts functional outcomes after minimally invasive surgical evacuation based on imaging data alone,” says Ahmed Kashkoush, MD, first author of the study and a neurosurgery resident at Cleveland Clinic. “It does so with accuracy similar to that of the ICH score, and it improves upon it when combined with other patient factors. This model helps answer the key question when we see one of these patients: Are they likely to benefit from surgery for this high-risk condition?”
Evidence is scant on how basal ganglia ICH should be treated — i.e., with surgical evacuation (using either standard or minimally invasive techniques) or medical management. Although relieving pressure through minimally invasive surgical evacuation appears to offer advantages over standard surgery, it’s unknown whether any method of hemorrhage evacuation for basal ganglia ICH leads to an outcome better than what’s possible with optimal medical management.
Selection criteria for surgery are currently poorly defined. Prediction tools to guide management — including the ICH score, which was developed based on combined populations of patients with lobar, basal ganglia and infratentorial bleeds — may not be valid specifically for ICH in the basal ganglia, owing to the basal ganglia’s compact neuroanatomy with multiple eloquent structures.
The Cleveland Clinic researchers designed their study to determine whether basal ganglia bleed morphology can help predict which patients might benefit from treatment with minimally invasive hemorrhage evacuation.
Advertisement
The study population consisted of 45 patients (62% men, median age of 53 years) who underwent minimally invasive surgical evacuation of a basal ganglia hemorrhage at Cleveland Clinic between 2013 and 2024. Median follow-up was approximately four months.
Two major factors were incorporated into heat maps:
Comparing the “good outcome” heat map to the “poor outcome” heat map enabled investigators to discern areas most likely to be specific to good or poor functional outcomes. The map for each patient was compared with the combined map for all other patients to validate the model.
The following hemorrhage patterns were found to be most predictive of outcome following minimally invasive surgical evacuation:
Based on imaging data alone, prognostic accuracy of the model was assessed using area under the receiver operating characteristic curve (AUC). The model’s AUC of 0.87 (95% CI, 0.76-0.97) was comparable to the AUC of the ICH score — i.e., 0.82 (95% CI, 0.71-0.97) — which is based on multiple factors.
Advertisement
Other factors predictive of poor outcome were older age, larger ICH volume and higher modified Graeb scale score (used to assess intraventricular hemorrhage severity), which are all derivative ICH score subcomponents. These and other preoperative variables, when included in a multivariate logistic regression model, predicted poor functional outcome significantly better than the ICH score.
Dr. Kashkoush notes that due to the study’s small size and single-center, retrospective design, its findings need further validation before the model can be incorporated into clinical practice. “The fact that there are multiple ways to evacuate a hemorrhage increases the complexity of discerning optimal surgical management,” he adds.
In the future, findings gleaned from the model — or an automated version that could be incorporated into individual clinical assessment — could serve as a useful prognostication tool. Dr. Kashkoush says an automated model could be created using deep-learning imaging methods and potentially integrated with the medical record.
“This study resulted in significant and intriguing findings that could help clinicians determine the important question of which patients presenting with a basal ganglia bleed would likely benefit from acute relief of mass effect,” notes senior author Mark Bain, MD, MS, a Cleveland Clinic vascular neurosurgeon who says he knows of no other researchers using modeling with basal ganglia ICH volumetric morphology to predict outcomes. “This method could also be applied to assist in prognostication for other brain hemorrhages.”
Advertisement
According to Dr. Bain, multicenter prospective clinical trials addressing optimal management of basal ganglia bleeds would be valuable. Using the model’s findings to help create comparable cohorts could greatly assist in future trial design, he adds.
The investigative team has expanded their research to retrospectively compare outcomes of model-identified comparable patients who underwent either medical management or surgical evacuation. Results are expected to be published shortly.
Advertisement
Advertisement

ENRICH trial marks a likely new era in ICH management

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Paired blood and brain tissue methylation findings raise prospect of noninvasive precision diagnosis

Quick and aggressive responses to multiple complications have led to remarkable recovery

Case series links catastrophic outcomes to therapy initiation within 48 hours post-procedure

Scientific program chair reflects on what may resonate longest from this year’s neurosurgery conference

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests