Applications, outcomes and untapped potential

Following Food and Drug Administration (FDA) approval in 2018, a novel purpose-built single-port (SP) robotic platform has been increasingly utilized for various procedures, both in urology and across other surgical specialties.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As the first institution to perform an SP procedure in the United States, Cleveland Clinic’s Glickman Urological Institute has been instrumental in pioneering innovative, regionalized surgical approaches, recently accomplishing an important milestone of surpassing 1,000 SP urological cases.
Jihad Kaouk, MD, Director of the Center of Advanced Robotic and Image-Guided Surgery at Cleveland Clinic’s Glickman Urological Institute, emphasizes that “single-port is not about one incision, and it is not about replacing the multi-port, rather it is about regionalizing our surgical field to the pathology area and minimize discomfort for our patients.”
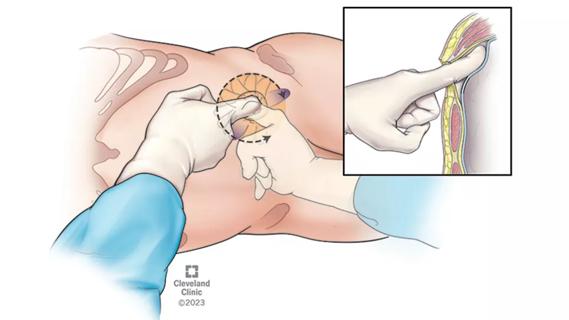
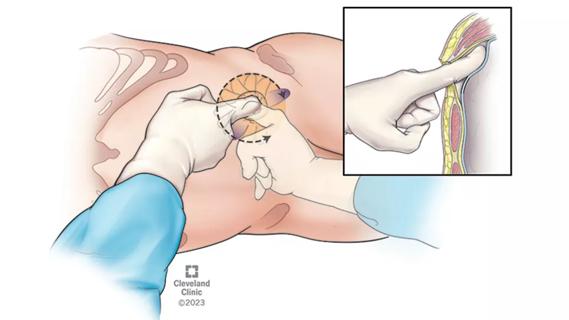
The SP robotic platform is unique given the narrow profile of the single robotic arm, which can simultaneously accommodate three double-jointed robotic instruments and a flexible high-definition camera. All these instruments can be introduced through a single 3 cm incision, as facilitated by a purpose-built surgical access port.
Compared to the conventional multi-port robotic platform, the SP platform offers improved maneuverability and ergonomics, especially when performing procedures in smaller and shallow surgical working spaces.
Working in a small surgical area facilitated the subsequent introductions of the transperineal and transvesical prostatectomy as well as the novel low anterior access (LAA) incision for various extraperitoneal kidney procedures.
Overall, the SP robot has facilitated multi-quadrant transperitoneal, extraperitoneal, retroperitoneal, transvesical, and transperineal access for a range of surgeries, including extraperitoneal kidney transplantation and autotransplantation, nephrectomy, pyeloplasty, prostatectomy, cystectomy as well as urinary tract reconstruction.
Advertisement
Cleveland Clinic was instrumental in the developmental phase of the SP robot system. After obtaining Institutional Review Board (IRB) approval in 2011, Dr. Kaouk and his team performed the first-in-human SP procedures in collaboration with Professor Villers in Lille, France. This included SP nephrectomy, SP partial nephrectomy and SP radical prostatectomy.
Then, after receiving the first clinical SP robotic system in the United States in September 2018, Cleveland Clinic’s team described the floating docking technique that significantly enabled SP procedures in shallow areas and performed several first-in-human SP procedures, including:
The team also has helped expand clinical indications for certain procedures, such as performing radical prostatectomy in patients with a hostile abdomen and with patients awake under epidural anesthesia without mechanical ventilation.

The opportunity to regionalize our surgical approach using the purpose-built SP platform has translated to substantive benefits towards enhancing patient comfort and minimizing perioperative morbidity.
Advertisement
Our team has demonstrated the utility of various novel, regionalized SP approaches, such as with the transvesical prostatectomy and low anterior access (LAA) retroperitoneal upper and lower tract procedures, in achieving same-day discharges in up to 92% with minimal postoperative pain, thus eliminating the need for opioid prescriptions in up to 98% of our cases.
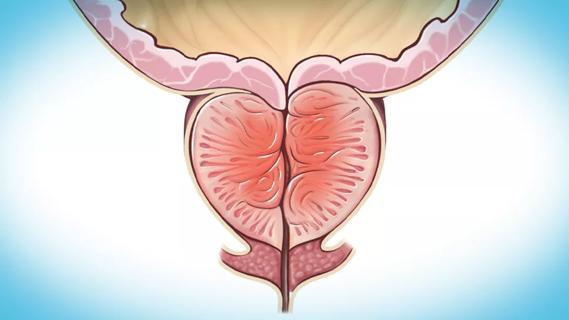
Furthermore, the ability to complete all surgical steps of transvesical radical prostatectomy entirely from within the confines of the bladder provided the opportunity to preserve the surrounding anatomy, including the external urinary sphincter and the supporting structures of the bladder.
These translated to the additional benefits of earlier return of urinary continence, with 40% achieving immediate continence following urinary catheter removal. The preservation of the peritoneum also confers additional benefits in reducing the risk of bowel complications, such as postoperative ileus, as well as minimizing the risk of postoperative incisional hernia, hence allowing patients an earlier return to their normal activities as soon as two weeks following their respective surgery.
In addition to the advantages of the SP in promoting regionalized surgical approaches, the unique features of the purpose-built platform also allow for added flexibility and maneuverability for multi-quadrant access from a single anatomical pivot point. This distinctive ability paved the way for the implementation of novel techniques, with a notable example including SP kidney autotransplantation, which involves the completion of two separate procedures (nephrectomy and transplantation) from a single transumbilical incision site. The procedure has since been utilized for various indications, including for the management of Nutcracker syndrome.
Advertisement

With new SP procedures continuing to be described and with many new centers across the country joining the SP program, there is a growing need to conduct various clinical studies and develop evidence-based guidelines on a large multi-institutional level.
“Any new innovations need to demonstrate value for our patients and our healthcare system,” says Dr. Kaouk, who established the Single-Port Advanced Research Consortium (SPARC) in 2018.
The collaborative group has since grown to include data-sharing agreements with 27 institutions and with an additional three more in progress, continuing its mission to drive important multi-institutional studies as reflected by the various peer-reviewed publications and presentations in national and international medical congresses.
While the novel purpose-built SP platform represents a significant advancement that opened a new frontier within the domains of minimally invasive surgery in urology, it is important to always remember the driver behind these innovations.
“It is important to remember that the robot is just a tool, and you have to pick the approach that best fits you, your experience, your patient, and the specific pathology,” says Dr. Kaouk.When beginning to offer SP robotic surgery, centers often face a steep learning curve. A robotic surgeon needs to perform appropriate SP training and proctoring.
References
Advertisement
Advertisement

First single-port renal vein transposition reduces recovery time and improves outcomes

Approach offers a ‘middle ground’ between radical prostatectomy and active surveillance
The low anterior access approach using the single-port robot is gaining attention within the field

Medical management remains the starting point for most symptomatic patients seeking treatment
Review the advantages and disadvantages of newer interventions
Pioneering and refining the approach in pyeloplasty, nephrectomy and more

More on the procedure and the institutional experience

Historic collaboration connects two Cleveland Clinic locations, enables real-time sharing of metrics and surgical progress