Targeted mRNA blocking could be first effective approach specific to this cardiovascular risk factor
A single injection of a short interfering RNA (siRNA) that inhibits hepatic production of a structural component of lipoprotein(a) (Lp[a]) was well tolerated and associated with reductions of up to 98% of this hard-to-address cardiovascular risk factor.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
These findings, from the phase 1 APOLLO trial in 32 adults with high baseline Lp(a) levels, were presented in a late-breaking clinical trials session at the American College of Cardiology’s Scientific Session on April 3 and published simultaneously in JAMA.
“The trial’s positive results support further development of this novel strategy for patients with elevated Lp(a),” says the study’s principal investigator, Steven Nissen, MD, Chief Academic Officer of Cleveland Clinic’s Heart, Vascular & Thoracic Institute. “If results continue to be positive, this agent could become a useful treatment for this inherited condition that confers such high cardiovascular risk.”
Elevated Lp(a) is a known independent risk factor for atherosclerotic cardiovascular disease and aortic valve stenosis, with about 20% of the population having plasma levels above 60 mg/dL. Those with levels above 140 mg/dL face a lifetime risk of cardiovascular disease similar to patients with familial hypercholesterolemia.
“Lp(a) levels are genetically determined, and lifestyle modifications that reduce other cardiovascular disease risk factors do not affect it,” notes study co-author Leslie Cho, MD, Section Head of Preventive Cardiology at Cleveland Clinic. “Although niacin and PCSK9 inhibitors can provide modest reductions of elevated Lp(a), there is no FDA-approved medical therapy to address it.”
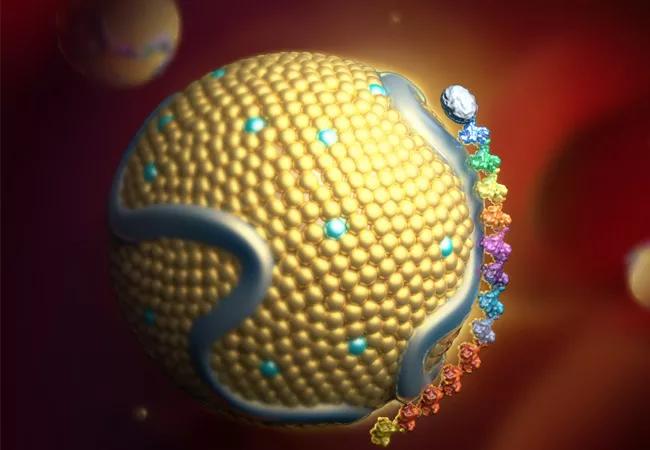
Various RNA-targeted therapies to block hepatic production of apolipoprotein(a), a key component of Lp(a), have been under investigation in recent years. This study employed an siRNA known as SLN360, which binds and degrades the mRNA produced by the LPA gene that encodes for apolipoprotein(a), reducing its production.
Advertisement
This first in-human trial using SLN360, conducted at five medical centers in three countries in collaboration with the Cleveland Clinic Coordinating Center for Clinical Research (C5Research), enrolled 32 adults with an Lp(a) concentration of at least 150 nmol/L and no known cardiovascular disease. The mean age of participants was 50 ± 13.5 years (53% female).
Participants were randomly assigned to one of four cohorts to receive a single subcutaneous injection of SLN360 (30 mg, 100 mg, 300 mg or 600 mg). Two participants in each cohort were randomly assigned to saline placebo. The investigators, study participants and sponsor were blinded to the randomization.
Patients were followed on days 7, 14, 30, 45, 60, 90 and 150 following injection. At each visit, safety was assessed and blood samples were obtained for Lp(a) and other laboratory values.
The primary efficacy assessment was the effect of SLN360 on plasma Lp(a) from baseline to 150 days. Key efficacy findings included the following:
Advertisement
Indicators of hepatotoxicity were also measured. One patient who received the 30-mg dose had a transient threefold elevation of the liver enzymes alanine aminotransferase and aspartate aminotransferase with no elevation in bilirubin; this may have been caused by the patient receiving a COVID-19 vaccination near this time.
No other indicators of liver dysfunction or other serious adverse events were observed. The most common adverse events were low-grade injection site events and headache.
Dr. Nissen notes that blocking translation of target proteins through RNA interference is a strategy that is increasingly being explored for drug development. “siRNA therapeutics have the potential to offer very specific treatment with a long duration of effect,” he says. “This study provides support that this strategy is potentially fruitful for targeting elevated Lp(a).”
He adds that larger and longer studies are needed to further evaluate safety and duration of effects of SLN360 on Lp(a). Cleveland Clinic is currently participating in a randomized, placebo-controlled study of multiple ascending doses of SLN360 to assess effects among patients with elevated Lp(a) and stable atherosclerotic cardiovascular disease over 201 days of follow-up (NCT04606602). Results are expected next year.
“We are very encouraged by the APOLLO trial results showing robust and sustained Lp(a) reduction with SLN360,” Dr. Nissen concludes. “We hope that further testing of this class of therapies will prove to reduce the consequences of Lp(a) in the clinical setting.”
Advertisement
The study was funded by Silence Therapeutics, which is developing SLN360.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more