Small interfering RNA lowered lipoprotein(a) by 94% during six-month follow-up after a single dose
In a phase 2 trial, the small interfering RNA lepodisiran reduced time-averaged levels of lipoprotein(a) (Lp[a]) by 93.9% from day 60 to day 180 following a single 400-mg dose, with no major safety concerns.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“These findings demonstrate that lepodisiran is a very effective therapy for Lp(a) lowering, providing high levels of reduction with long durability,” says lead investigator Steven Nissen, MD, who reported the results in a late-breaking science portion of the American College of Cardiology Scientific Session. The study was published simultaneously in the New England Journal of Medicine.
In addition to the above-noted reduction at 180 days, 400 mg of lepodisiran lowered Lp(a) levels from day 30 to day 360 by 88.5% after a single dose and by 94.8% after two doses (given at baseline and at day 180). Moreover, Lp(a) levels remained 53.4% below baseline at 540 days (18 months) after a single dose and 74.2% below baseline at 360 days after a second dose.
“The extended duration of lepodisiran will allow infrequent dosing in an ongoing phase 3 cardiovascular outcomes trial of this agent,” says Dr. Nissen, Chief Academic Officer of Cleveland Clinic’s Heart, Vascular and Thoracic Institute.
Dr. Nissen notes that the Cleveland Clinic Coordinating Center for Clinical Research (C5Research) is coordinating trials of several of the five investigational therapies in clinical development for Lp(a) reduction, which gives him considerable familiarity with these therapies. He says lepodisiran has demonstrated the most durable Lp(a) lowering of all of these agents, an observation believed to be related to its unique chemical structure, which gives rise to its designation as a noncanonical small interfering RNA.
Advertisement
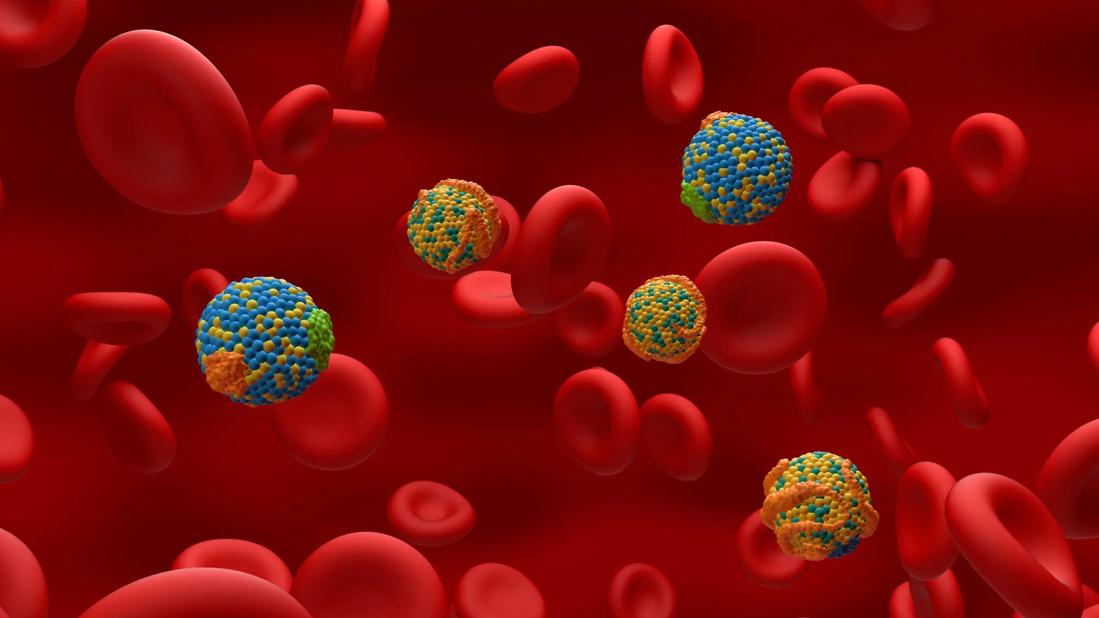
Like other nucleic acid-based therapies developed for Lp(a) reduction, lepodisiran was designed to degrade the hepatic messenger RNA that codes for apolipoprotein(a). Its double-stranded RNA structure is notable for a hairpin-like component known as a tetraloop that connects the RNA strands. Lepodisiran is a substrate for an enzyme known as Dicer that cleaves the structure into the active small interfering RNA, which may enhance effectiveness. “The tetraloop also affords stability,” Dr. Nissen explains. “As a consequence of its structure, lepodisiran has an Lp(a)-lowering effect that’s more durable than that of previously studied drugs.”
Developers of lepodisiran and the other agents are aiming to address an unmet need for treatments for elevated Lp(a), which is associated with a heightened risk — and often an accelerated course — of atherosclerotic cardiovascular disease and aortic stenosis. Approximately 20% to 25% of the population has elevated blood levels of Lp(a) — i.e., >125 nmol/L. Elevated Lp(a), which is largely attributable to variations in the LPA gene that encodes apolipoprotein(a), is not meaningfully reduced by available lipid-lowering therapies or lifestyle modifications.
The phase 2 trial of lepodisiran follows a phase 1 study in which the highest dose assessed — 608 mg — reduced Lp(a) serum levels by more than 90% for 337 days after a single injection. “We undertook the phase 2 study to further evaluate lepodisiran’s safety in a larger population with higher Lp(a) levels, better define the magnitude and duration of Lp(a) reduction, and inform the optimal dose and dosing interval for a multiyear phase 3 cardiovascular outcomes trial,” Dr. Nissen notes.
Advertisement
The study included 320 adults aged 40 or older with Lp(a) serum concentrations of 175 nmol/L or higher. Participants were treated at 66 centers in North America, Europe, Asia and South America.
Participants were randomized in a 1:2:2:2:2 ratio to receive the following at baseline and day 180:
Randomization was stratified by baseline Lp(a) level and the presence or absence of high cardiovascular risk. All treatments were given by subcutaneous injection. Efficacy and safety data were collected over 540 days of follow-up.
The two groups that received lepodisiran 400 mg at baseline (n = 141) were pooled for the primary analysis. The primary end point was the placebo-adjusted percentage change from baseline in time-averaged Lp(a) level from day 60 to day 180.
The median baseline Lp(a) level across the cohort was 253.9 nmol/L. Mean participant age was 62.7 years. Forty-three percent of participants were women, 68% met the criteria for being at high risk for a cardiovascular event and 48% had known coronary artery disease. Results on the primary end point are shown the table below.
| Group | Change in time-averaged Lp(a) from days 60 to 180 | 95% confidence interval |
|---|---|---|
| Placebo + placebo (n = 69) | — | — |
| Lepo 16 mg + 16 mg (n = 36) | –40.8% | –55.8% to –20.6% |
| Lepo 96 mg + 96 mg (n = 74) | –75.2% | –80.4% to –68.5% |
| Lepo 400 mg + placebo and lepo 400 mg + 400 mg (pooled) (n = 141) | –93.9% | –95.1% to –92.5% |
| Group | ||
| Placebo + placebo (n = 69) | ||
| Change in time-averaged Lp(a) from days 60 to 180 | ||
| — | ||
| 95% confidence interval | ||
| — | ||
| Lepo 16 mg + 16 mg (n = 36) | ||
| Change in time-averaged Lp(a) from days 60 to 180 | ||
| –40.8% | ||
| 95% confidence interval | ||
| –55.8% to –20.6% | ||
| Lepo 96 mg + 96 mg (n = 74) | ||
| Change in time-averaged Lp(a) from days 60 to 180 | ||
| –75.2% | ||
| 95% confidence interval | ||
| –80.4% to –68.5% | ||
| Lepo 400 mg + placebo and lepo 400 mg + 400 mg (pooled) (n = 141) | ||
| Change in time-averaged Lp(a) from days 60 to 180 | ||
| –93.9% | ||
| 95% confidence interval | ||
| –95.1% to –92.5% |
Corresponding changes from day 30 to day 360 were as follows:
| Group | Change in time-averaged Lp(a) from days 30 to 360 | 95% confidence interval |
|---|---|---|
| Placebo + placebo (n = 69) | — | — |
| Lepo 16 mg + 16 mg (n = 36) | –41.2% | –55.4% to –22.4% |
| Lepo 96 mg + 96 mg (n = 74) | –77.2% | –81.8% to –71.5% |
| Lepo 400 mg + placebo (n = 72) | –88.5% | –90.8% to –85.6% |
| Lepo 400 mg + 400 mg (n = 69) | –94.8% | –95.9% to –93.4% |
| Group | ||
| Placebo + placebo (n = 69) | ||
| Change in time-averaged Lp(a) from days 30 to 360 | ||
| — | ||
| 95% confidence interval | ||
| — | ||
| Lepo 16 mg + 16 mg (n = 36) | ||
| Change in time-averaged Lp(a) from days 30 to 360 | ||
| –41.2% | ||
| 95% confidence interval | ||
| –55.4% to –22.4% | ||
| Lepo 96 mg + 96 mg (n = 74) | ||
| Change in time-averaged Lp(a) from days 30 to 360 | ||
| –77.2% | ||
| 95% confidence interval | ||
| –81.8% to –71.5% | ||
| Lepo 400 mg + placebo (n = 72) | ||
| Change in time-averaged Lp(a) from days 30 to 360 | ||
| –88.5% | ||
| 95% confidence interval | ||
| –90.8% to –85.6% | ||
| Lepo 400 mg + 400 mg (n = 69) | ||
| Change in time-averaged Lp(a) from days 30 to 360 | ||
| –94.8% | ||
| 95% confidence interval | ||
| –95.9% to –93.4% |
Waterfall plot analysis showed highly consistent levels of substantial Lp(a) reduction across almost all patients in the pooled 400-mg dose groups.
Secondary endpoints included placebo-adjusted apolipoprotein B serum concentrations, as reductions in these levels are consistently associated with positive effects on major cardiovascular events. These levels showed dose-dependent maximal reductions with lepodisiran therapy, from 2.8% with doses of 16 mg dose to 15.5% with two doses of 400 mg. The investigators note, however, that it is uncertain whether reductions in apolipoprotein B with nucleic acid-based therapies for Lp(a) will contribute to clinical benefit.
Advertisement
Safety findings were favorable, with no reports of serious adverse events related to the study drug. Transient and generally mild injection-site reactions were reported in 0% to 11.6% of participants, following a dose-dependent pattern.
“These findings indicate that lepodisiran can be given very infrequently and still produce very durable reductions in Lp(a),” Dr. Nissen says. “We can now adapt the ongoing phase 3 outcomes trial to use the optimal dose and dosing interval based on these findings.”
He notes that the phase 3 trial (ACCLAIM-Lp(a), NCT06292013), which is enrolling 12,500 participants, will be the first phase 3 investigation of an Lp(a)-lowering therapy to include primary prevention patients in addition to secondary prevention patients. “Most of the 1.4 billion people in the world with elevated Lp(a) haven’t yet had a cardiovascular event, so phase 3 trials of these therapies in a primary prevention setting are quite important,” Dr. Nissen says.
He adds that the phase 3 trial, in which Cleveland Clinic will be a participating center, is already well underway. “Lepodisiran’s unique chemical structure and durable Lp(a) reduction in the phase 1 study prompted initiation of the phase 3 cardiovascular outcomes trial before the phase 2 study was completed,” he says. However, even with the phase 3 study’s swift initiation, results are several years off.
Meanwhile, Dr. Nissen and his coinvestigators acknowledge a couple of limitations of the phase 2 study. One is that Black participants made up only 2% of the study cohort even though elevated Lp(a) is more common in Black people than in other racial groups. “Further study in this population will be necessary,” the authors write in their study report.
Advertisement
Additionally, the phase 2 study administered no more than two doses of lepodisiran, leaving the effect of additional doses uncertain. “The long duration of action of a drug like this presents a conundrum for researchers,” Dr. Nissen says. “Conventional wisdom in pharmacology is that it takes five half-lives to reach a medication’s steady state. This suggests the phase 2 study probably didn’t even achieve steady state of lepodisiran, but we didn’t want to needlessly delay the start of phase 3 testing of a therapy that so effectively reduces Lp(a). The reduction might be even larger if steady state is reached after additional doses, but that’s something we’ll need to determine from the ongoing phase 3 trial.”
“This is an exciting time in Lp(a) research, with an antisense oligonucleotide agent, several small interfering RNA agents, and one Lp(a)-lowering oral medication all in clinical trials,” adds Leslie Cho, MD, Co-Section Head of Preventive Cardiology at Cleveland Clinic. “We eagerly await results of the cardiovascular outcomes trials to learn whether lowering Lp(a) lowers cardiovascular risk.”
The study was supported by Eli Lilly, which is developing lepodisiran.
For more from Dr. Nissen on lepodisiran and this study's findings, listen to the below episode of Cleveland Clinic's weekly Cardiac Consult podcast.
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2237537/16889250)
Advertisement

Yet 21.4% of tested individuals had Lp(a) elevation
Phase 2 trial of zerlasiran yields first demonstration of longer effect with each dose of an siRNA
It's time to increase testing for this major cardiovascular risk factor in advance of new therapies

Undetectable levels achieved for nearly nine months in phase 1 trial

First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3

Proteins related to altered immune response are potential biomarkers of the rare AD variant

Resourceful approaches to the care of patients with microvascular disease and elevated Lp(a)

Scenarios where experience-based management nuance can matter most