Intra- and postoperative technologies make a difference
By Aleksandra Rachitskaya, MD, Alex Yuan, MD, PhD, and Meghan DeBenedictis, MS, LGC, MEd
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 66-year-old male came to the Cole Eye Institute for an eligibility evaluation for the Argus II retinal prosthesis system. He and his wife were anxious. He was diagnosed with retinitis pigmentosa when he was 10 years old and has lost his vision completely in the past seven years. Despite being completely blind, he was hoping for a chance to enjoy some vision again.
The Cole Eye Institute has rapidly become the leader in Argus II implantation since the first retinal implant surgery at Cleveland Clinic was performed in the summer of 2015. The Argus team, led by retina surgeons Aleksandra Rachitskaya, MD, and Alex Yuan, MD, PhD, as well as Meghan DeBenedictis, MS, LGC, MEd, has implanted the highest number of prostheses in North America and has developed innovative research initiatives that advance the understanding of how the device works and how the patient experience can be improved.
The Argus II retinal prosthesis system (Second Sight Medical Products, Inc, Sylmar, CA), the team explained to the potential Argus II recipient, is approved for patients with bare light perception or worse vision in both eyes due to retinitis pigmentosa. The prosthesis provides artificial vision, which can help with independence, orientation, mobility and social integration.
Following an eligibility evaluation, the patient was scheduled for surgery and postoperative rehabilitation.
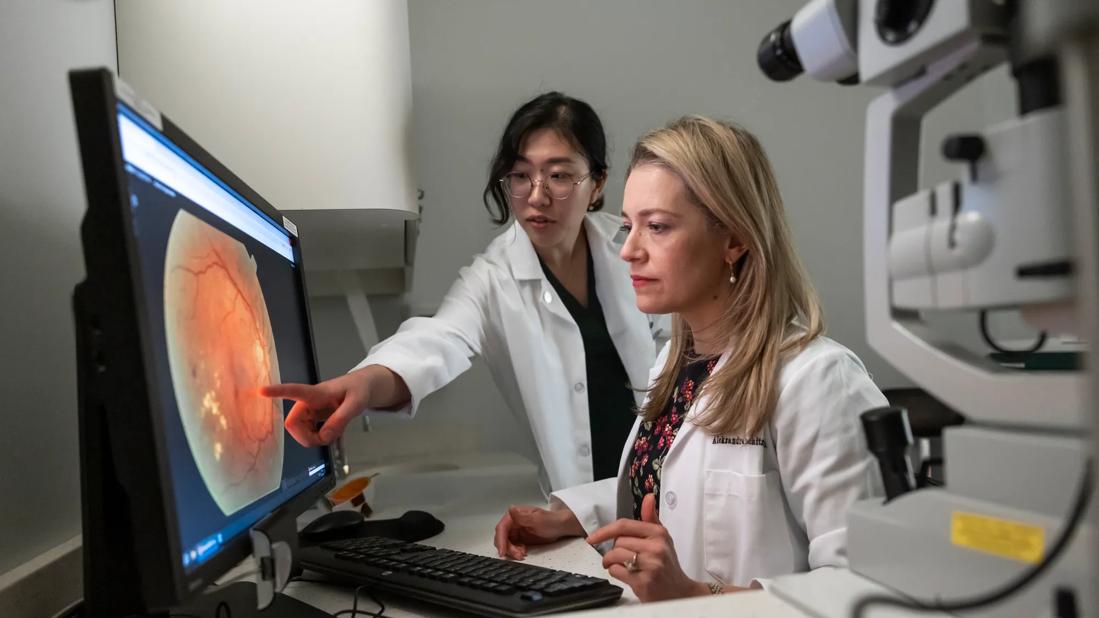
To optimize the retinal prosthesis array placement, the Cole Eye Argus II team used intraoperative optical coherence tomography (i-OCT). Cole Eye Institute is one of a few centers that routinely uses i-OCT, which allows for visualization of the implant-retina interface before, during and after the implant array is secured to the macula with the use of a specially designed tack.1 It allows for optimal placement of the Argus II array and may translate into better visual outcomes.
Advertisement
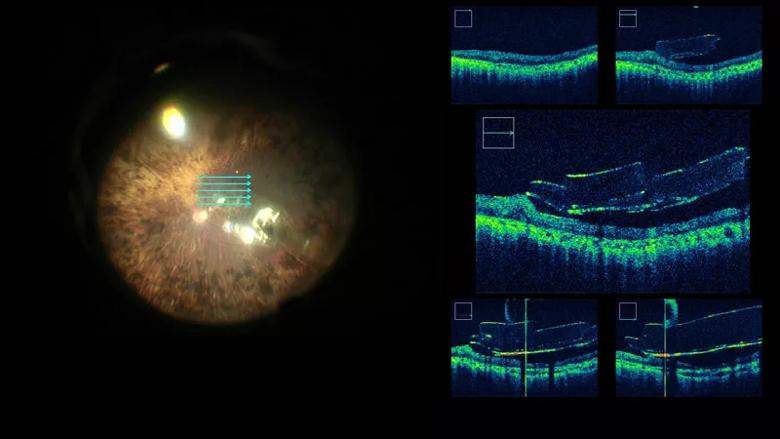
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c2146cd9-da44-4e5b-a9f9-0299c38e8b99/18-EYE-4339-Argus-CQD-inset_jpg)
Intraoperative optical coherence tomography of the Argus II array
To facilitate communication during surgery, the surgeons used a three-dimensional (3D) visualization system (Ngenuity, Alcon, Fort Worth, TX), which allows everyone in the operating room to experience the same surgical views. Argus II implantation surgery involves several steps which greatly benefit from this technology as described by a recent publication by the Cole Eye Argus II team.2 For example, creation of the sclerotomy for introduction of the array into the vitreous cavity and the intraocular work including array tacking was greatly enhanced using the 3D system.
One of the key components of being able to use the Argus II system successfully is post-implant rehabilitation and training. However, the standard approach might not be effective for everyone. This Argus II recipient had a difficult time interpreting the visual stimulation he was experiencing. In collaboration with Jay Alberts, PhD, from the Cleveland Clinic Lerner Research Institute Department of Biomedical Engineering, the Cole Eye Argus II team investigated the role of computer-assisted rehabilitation in Argus II recipients.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/daee84b4-2c5d-4aa8-9d26-6e04b0fd54cd/18-EYE-4339-Argus-CQD-inset-2_jpg)
The Computer Assisted Rehabilitation ENvironment (CAREN) (Motekforce Link, Amsterdam, Netherlands) consists of a 10-camera motion capture system (Vicon Inc., Oxford, UK), D-Flow control software (Motekforce Link) with a 180° curved projection screen and a six-degree-of-freedom motion platform and treadmill. It simulates a variety of environments while the patient is using the Argus II system in the safety of a monitored setting. The patient was able to train with the Argus II system while safely ambulating on a treadmill using virtual reality.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b0d699eb-fae9-40fe-9454-bacb20d819c0/18-EYE-4339-Argus-CQD-Feat-new_jpg)
Following this four-week training protocol, the patient reported having more confidence in moving around, increased motivation to use the Argus II, an improved ability to scan while walking and improved balance. The Cole Eye Institute is the only Argus implantation facility to offer this unique virtual reality experience.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/02208812-85af-4360-ab59-32bc2e39dd6a/18-EYE-4339-Argus-CQD-inset-3_jpg)
This patient, like many other Cole Eye Institute patients, benefited from the Argus II implant. This was possible not only due to the Argus II system itself, but due to the novel technologies that the Argus II team at the Cleveland Clinic Cole Eye Institute is continuously working on with its many collaborators.
These new technologies offer hope of improving vision provided by a retinal prosthesis. This hope is essential to patients with retinal degeneration, many of whom were previously told they were going blind and had no treatment options.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift