Surgical drainage yields excellent results
By Jeffrey M. Goshe, MD; Gabrielle Yeaney, MD; and Arun D. Singh, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
About one year prior to presenting in our department, a 17-year-old girl noticed a painless “red spot” affecting the inferior bulbar surface of her right eye. An outside ophthalmologist examined her and noted a small prominent conjunctival vessel inferiorly with prominent, circumferential cystic lymphatic changes. The lesion remained stable for nine months, but then suddenly and dramatically enlarged.
When she presented for evaluation at Cleveland Clinic Cole Eye Institute, we found no evidence of trauma or recent viral illness. She did not wear contact lenses. She had a remote seizure disorder, successfully managed with oral levetiracetam for five years. Her vision was 20/20 OU, intraocular pressure was 18 and 22 mm Hg, and other eye exam measures were all within normal limits. However, slit-lamp examination demonstrated a large circumferential network of blood-filled vessels extending from the limbus in a 4-8 mm wide zone (Figures 1A, B). The superficial vessels were freely mobile, but deeper vessels were fixed.
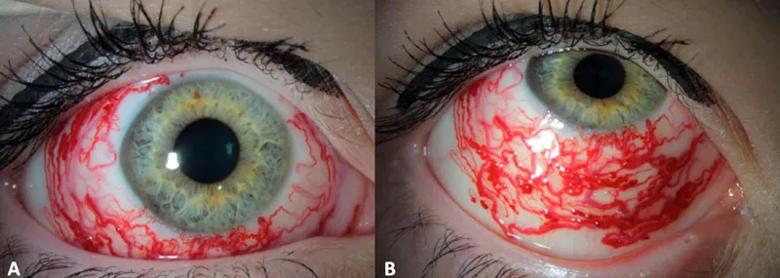
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/16f6ca9c-f0d4-411c-a6d1-dcde3117f5c5/16-EYE-2702-HC-Surgery-CQD-Inset-1_jpg)
FIGURE 1. A and B, Slit-lamp photographs demonstrating appearance of prominent circumferential vessels.*
Magnetic resonance imaging and MRI angiography of the brain and orbits, ordered based on her seizure history, proved normal. Anterior segment fluorescein angiography revealed normal filling of surrounding conjunctival arterioles and venules. However, the angiogram did confirm no-flow sequestration of blood in lymphatic channels, confirming our suspicion of the lymphatic origin of channels, and we diagnosed nonresolving lymphangiectasia haemorrhagica conjunctivae (LHC).
Advertisement
LHC is a rare condition that occurs as a result of acute or subacute hemorrhagic engorgement of conjunctival lymphatic channels. How blood enters the channels is not well understood. Some think it is a matter of valve malfunction that allows retrograde flow from venous vessels. It generally affects only one quadrant; circumferential cases are rare. LHC tends to be self-limiting, resolving over days to weeks, but some patients experience multiple episodes.
Because LHC lesions are usually minimally disfiguring, ophthalmologists manage them conservatively. If they progress, laser cautery can be used.
Our case was unusual in terms of severity and chronicity. Without evidence of visible feeding vessels, we bypassed the laser cautery option and decided that surgery offered the best chance for a good cosmetic outcome. The patient and her family agreed. The technique had not been used for LHC before, but our colleagues had described its use for surgical excision of symptomatic lymphangiectasis (nonhemorrhagic).
The procedure, performed under general anesthesia, began with an 8 mm temporal conjunctival incision. We noticed right away that some of the lymphangiectatic channels appeared less prominent and blood had drained from them. So instead of excising the conjunctiva as planned, we decided to make multiple small incisions and apply pressure with surgical sponges to drain channels. We did cauterize larger channels, and excised a 2 mm strip for histopathology. We closed the conjunctival flap with fibrin glue, applied a 22 mm bandage contact lens and instilled topical antibiotics and steroid eye drops.
Advertisement
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/Kpu0wk3yoPQ?feature=oembed)
The biopsy confirmed the LHC diagnosis. After two weeks, we removed the contact lens. Dilated lymphatic channels remain visible clinically and with optical coherence tomography, but are not evident to the normal observer (Figures 2A, B, C). The family, patient and her ophthalmology team are all very satisfied with the results and the patient has not experienced any recurrences after more than one year.
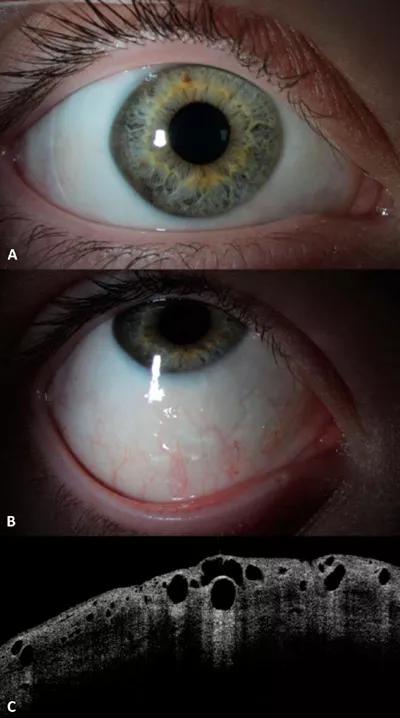
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/18832f1c-124a-4c31-9940-8159df95a787/16-EYE-2702-HC-Surgery-CQD-Inset-2_jpg)
FIGURE 2. A and B, Slit-lamp photographs demonstrating appearance four months after surgical drainage. Note the prominent conjunctival lymphatics visible inferiorly. C, Anterior segment optical coherence tomography showing persistent dilated conjunctival lymphatic channels.*
We were pleased at the relative ease with which blood could be drained from lymphatic channels using multiple incisions and manual drainage that also spared the surrounding conjunctiva and achieved good cosmesis. When spontaneous resolution does not occur in severe LHC, this technique could be an excellent alternative to offer patients.
Images and videos used with permission from Wolters Kluwer Health Inc.
Dr. Goshe is staff in the Cole Eye Institute. Dr. Yeaney is staff in the Pathology and Laboratory Medicine Institute. Dr.Singh is Director of the institute’s Department of Ophthalmic Oncology.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift