If you can’t see it, you can’t treat it
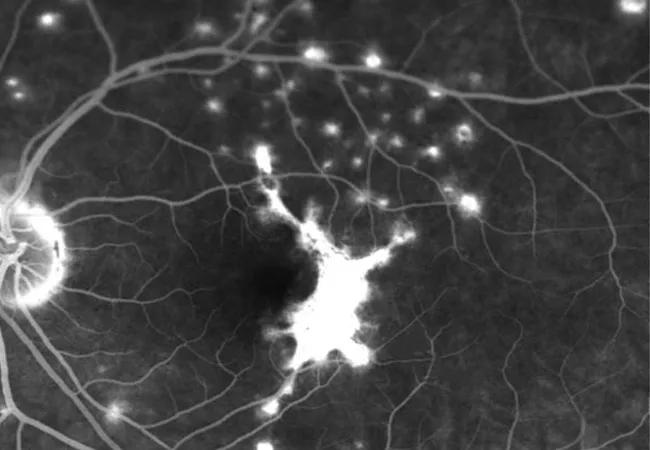
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/03d47eb8-dd7e-4aaf-9319-912ceff1ae15/16-EYE-2728-Srivastava-CQD-Hero_jpg)
16-EYE-2728-Srivastava-CQD-Hero
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Standard tools for diagnosing choroidal neovascularization (CNV) in uveitis, fluorescein angiography (FA) and optical coherence tomography (OCT), only provide part of the picture. Both can fail to distinguish between isolated inflammatory lesions and CNV, a crucial distinction. Plus, FA is invasive, and neither method is 100 percent reliable.
Thus, CNV can be very difficult to identify, particularly in patients with posterior uveitis who otherwise have good vision. CNV, if untreated, can lead to severe vision loss in patients with uveitis.
Optical coherence tomography angiography (OCTA) is a new imaging technology that allows us to noninvasively image retinal and choroidal vasculature and gives us the ability to acquire very high resolution images that are almost 3-D. It allows us to examine various layers of the retinal vasculature, providing a unique, detailed view of blood flow.
Having experienced OCTA’s usefulness in assessing CNV, we decided to formally investigate this emerging technology in identifying underlying CNV. Our results were published recently in the British Journal of Ophthalmology.
The prospective, descriptive case series involved 12 patients seen at Cole Eye Institute uveitis clinic between December 2014 and September 2015 with suspected punctate inner choroidopathy (PIC) and multifocal choroiditis and panuveitis (MCP) complicated by choroidal neovascular membranes. Nine were followed longitudinally, the longest nine months.
Detailed slit-lamp examinations were performed, along with posterior pole examination. Patients underwent conventional spectral domain OCT of the macula, and FA was obtained on five patients. Each patient underwent OCTA of the macula.
Advertisement
Patients ranged in age from 23 to 62 (mean 39 years old) and all were female.
Active CNV was suspected in 17 eyes of the 12 enrolled patients, and OCTA was able to identify findings suspicious for CNV membranes in 15 eyes of 11 patients. CNV appeared as a network of hyper-reflective vessels at the level of the choriocapillaris, sometimes extending into the outer retina (see Figures 1C, 1F and 2A). Seven had PIC and five had MCP.
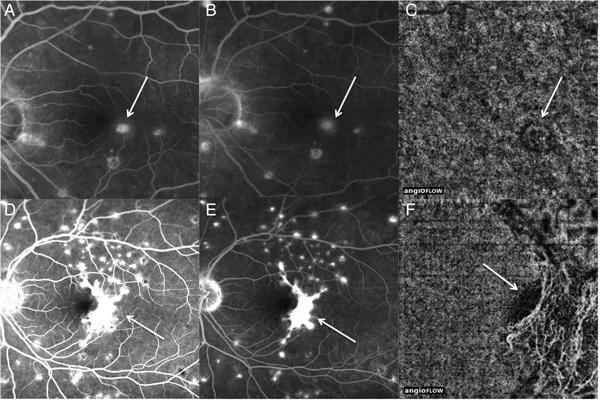
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/33a0b591-a35b-4e5a-850a-950c89a39069/16-EYE-2728_fig1-600p_jpg)
Figure 1 – Images of fluorescein angiography (FA) and corresponding optical coherence tomography angiography (OCTA) are shown. (A) Image showing the early FA in a patient with punctate inner choroidopathy. In the macula there is evidence of early staining (arrow). (B) In the late frame of the FA there is staining with mild leakage (arrow). There is no clear evidence to identify a choroidal neovascularisation (CNV) from an isolated inflammatory lesion. (C) The corresponding OCTA shows a small choroidal neovascular membrane that corresponds with the area of questionable leakage on FA (arrow). (D–E) The early and late frame FA of a patient with a known large CNV (arrow) is shown. (F) The OCTA shows an elaborate CNV that corresponds with the CNV on FA (arrow).
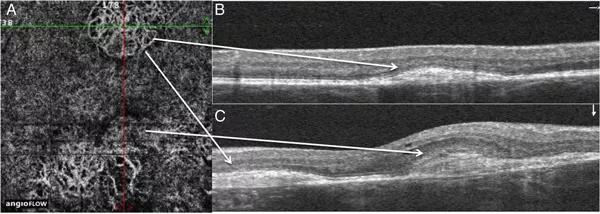
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/57d718fa-2264-4929-95aa-68b657b13b72/16-EYE-2728_fig2-600p_jpg)
Figure 2 – Optical coherence tomography (OCT) and OCT angiography (OCTA) images of a patient with multiple choroidal neovascularisation (CNV) are shown. (A) OCTA image of a patient with multiple CNV in the right eye is shown. The inferonasal aspect of the CNV has less distinct vessels compared with the more matured well-defined vessels of the CNV in other regions. Additionally, there is a ring of hypofluorescence around this inferonasal region of the CNV. (B) The horizontal OCT through the superior CNV on the OCTA shows a well-defined lesion that was thought to be clinically inactive. (C) Vertical OCT through the region of the less well-defined vessels shows hyper-reflective material in the outer retina as well as mild intra-retinal fluid. (Figures copyrighted by and reprinted with permission from the British Journal of Ophthalmology.)
Advertisement
Essentially, OCTA allowed us to identify all cases of CNV in this patient set, with the exception of one patient in whom the image was not performed in the correct area.. OCTA provided rich detail about the lesions compared with FA. In patients with simultaneous FA and OCTA, the OCTA identified the CNV in all cases, while FA missed it in half.
Of interest, FA sometimes does not differentiate well between blood vessel growth and inflammatory granuloma (which uveitis patients may experience) because of the similarity in appearance of the lesions. Given the difficulty of differentiating inflammatory lesions from early CNV on OCT and FA, OCTA may provide a valuable method of monitoring patients with posterior uveitis highly correlated with development of CNV.
Our paper helps show that OCTA can assist in early detection of complications in patients with PIC and MCP, specifically choroidal neovascularization.
The study demonstrated the power of this tool. We were able to observe changes in blood vessels over time with treatment. Early on, blood vessels look immature. As blood vessels fibrose with treatment, the blood vessel anatomy changes, becoming much more distinctive and signifying maturation. This is something we have only been able to visualize now, thanks to OCTA technology.
Our final finding pertains to OCT. OCT allows us to recognize various patterns of elevation in vessels that are indicative of CNV. When we see such changes on OCT, we should be suspicious of CNV and should examine patients further with either FA or OCTA.
Advertisement
The gist of our study is that in high-risk patients, such as those who have posterior uveitis, OCTA is a noninvasive tool that can be very beneficial in identifying complications early on, especially CNV, so that they can be treated appropriately and potentially preventing vision loss. Future OCTA studies may help us better understand disease pathology and response to therapy.
OCTA is becoming a standard imaging technology in uveitis subspecialty practices. Still, OCTA is only one of the imaging tools needed for assessing uveitis. It is not going to replace FA, but it will be another adjunct in the assessment of these patients.
Dr. Srivastava is a uveitis specialist on staff in the Cole Eye Institute. Careen Y. Lowder, MD, PhD, and Peter K. Kaiser, MD, co-authored this article.
Advertisement
Advertisement
A review of pathophysiology, risk factors, clinical presentation and treatment options
How computational tools and personalized biomechanics can improve keratoconus detection, ectasia risk assessment and surgical outcomes
Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma
Registry data highlight visual gains in patients with legal blindness
Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence
A look at emerging technology shaping retina surgery
A primer on MIGS methods and devices
7 keys to success for comprehensive ophthalmologists