Large longitudinal study supports earlier intervention over clinical surveillance
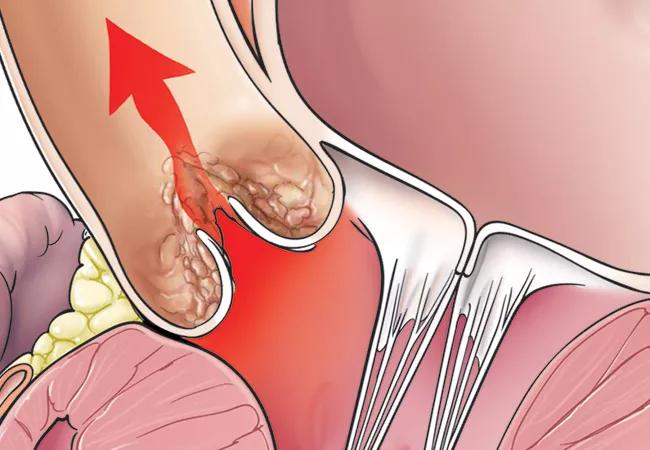
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a828070b-6c12-45d4-a33f-5b323f2a33de/20-HVI-1998310_aortic-stenosis_650x450-1_jpg)
stenosed aortic valve within the heart
Patients who undergo aortic valve replacement (AVR) for moderate aortic stenosis (AS) fare better, on average, than comparable patients managed with clinical surveillance, with significant improvements seen in survival and left ventricular remodeling over multiyear follow-up. So finds a retrospective analysis of more than 1,400 patients with moderate AS who were treated at Cleveland Clinic with AVR (either surgical [SAVR] or transcatheter [TAVR]) or managed with clinical surveillance. The study was published online in Open Heart.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We found a significant advantage to replacing the aortic valve in patients with moderate AS rather than waiting until symptoms became severe,” says senior and corresponding study author Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic. “Increasing evidence indicates that intervention is a promising alternative to conservative management in the setting of moderate AS.”
AS, increasingly seen in an aging population, is not treated with AVR per current guidelines except in patients with severe symptomatic disease or evidence of left ventricular systolic dysfunction, or in those with moderate AS who are undergoing open-heart surgery for another indication. Otherwise, surveillance is recommended every year or two for moderate AS until patients meet criteria for intervention.
However, over the past several years, multiple studies have shown that moderate AS has a poorer prognosis than previously thought, with a clear increased risk of heart failure, cardiovascular mortality and all-cause mortality.
Little has been published on intervention for moderate AS, consisting mostly of studies with small sample sizes and short follow-up times. This study was designed to compare long-term clinical outcomes and echocardiographic changes in such patients managed with either AVR or clinical surveillance, using real-world data from a large health system.
The analysis included 1,421 patients (mean age, 75.3 ± 5.4 years; 60% men) with moderate AS of the native valve (defined as an aortic valve area of 1.0-1.5 cm2 at index echocardiogram). Patients were selected from the Cleveland Clinic echocardiography database between 2008 to 2016 and followed until 2018 (median follow-up of 6 years).
Advertisement
Cohorts were categorized by the following management strategies:
Overall, 363 patients (25.5%) died during follow-up. Among them, 266 deaths (18.7% of the overall cohort) were classified as cardiovascular deaths.
Comparisons between the AVR and clinical surveillance groups revealed that intervention was associated with a lower risk of all-cause death (adjusted hazard ratio [HR] = 0.51; 95% CI, 0.34-0.77; P = .001) and cardiovascular death (adjusted HR = 0.50; 95% CI, 0.31-0.80; P = .004).
These outcomes were evident regardless of sex, receipt of other open-heart surgeries or underlying malignancy.
Survival benefits associated with AVR were significant only among patients with preserved (≥50%) left ventricular ejection fraction (LVEF), although there was a trend toward greater survival in patients with low LVEF. Dr. Kapadia notes that the small number of patients with reduced LVEF in the AVR cohort may have limited the findings. It is also possible, he adds, that patients with low LVEF already have cardiac damage that cannot be significantly remedied with AVR. “More study is needed of this important question,” he says.
Improved echocardiographic findings were also evident in patients who underwent AVR. In multivariable-adjusted analysis, they had significantly higher LVEF and lower right ventricular systolic pressure over time than patients managed with clinical surveillance, who worsened in both of those parameters over the study period.
Advertisement
Both TAVR and SAVR groups demonstrated significant benefit over clinical surveillance. Most AVR patients in the study had a surgical rather than transcatheter approach, reflecting the time period analyzed (2008-2016). Despite the small TAVR cohort size, a lower incidence of all-cause mortality was still evident in that group compared with clinical surveillance (adjusted HR = 0.45; 95% CI, 0.22-0.91; P = .026).
Several multicenter randomized controlled trials are currently underway comparing different TAVR devices against medical management for moderate AS: TAVR UNLOAD (NCT02661451), Evolut EXPAND TAVR II (NCT05149755) and PROGRESS (NCT04889872), with Cleveland Clinic participating in the first two trials.
“Our study findings, especially in light of treatment advances and increased understanding of the poor prognosis associated with moderate AS, make us more inclined to offer intervention to our patients earlier in the disease process,” Dr. Kapadia concludes. “I look forward to gaining more clarity from randomized controlled trials about identifying candidates and optimum timing for intervention.”
“Now that procedural mortality is low for both TAVR and SAVR in expert centers, the next frontier in research in aortic valve disease is determining the optimal time to replace the valve,” adds Brian Griffin, MD, Medical Director of Cleveland Clinic’s Valve Center, who was not involved in the study.
“It has become clear in a number of studies,” he continues, “that patients undergoing AVR do not always enjoy the survival benefit expected. This paper provides further insights into this phenomenon and raises the question of whether AVR should be performed at an earlier stage, at least at centers with outstanding procedural outcomes for SAVR and TAVR. Further studies are underway to try and address this important question.”
Advertisement
“With the development of minimally invasive techniques for SAVR, such as mini-thoracotomy and partial sternotomy, patients experience less pain, faster recovery, earlier discharge (as soon as three days) and smaller scars compared with traditional complete sternotomy,” adds cardiac surgeon Marijan Koprivanac, MD, MS, who also was not involved in the study. “Considering this, along with the proven durability of SAVR and less than 1% mortality at some centers of excellence, the discussion about intervening on moderate AS becomes much easier. Given these important findings, intervening on moderate AS seems justified, and using safe, minimally invasive techniques to improve patient experience and outcomes may help avoid progression of heart failure due to AS. This study is a significant step in unraveling the moderate stenosis enigma, but further studies and trials are necessary to continue demystifying moderate stenosis.”
Advertisement
Advertisement
JACC State-of-the-Art Review details current knowledge and new developments
Age and other factors figure into the choice among SAVR, TAVR, Ross, Ozaki and more
Optimally timed valve replacement depends on an expert approach to nuanced presentations
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Series of 145 patients characterizes scope of presentations, interventions and outcomes
Experience-based takes on valve-sparing root replacement from two expert surgeons
TVT Registry analysis could expand indication to lower surgical risk levels
New review distills insights and best practices from a high-volume center