How it helps patients
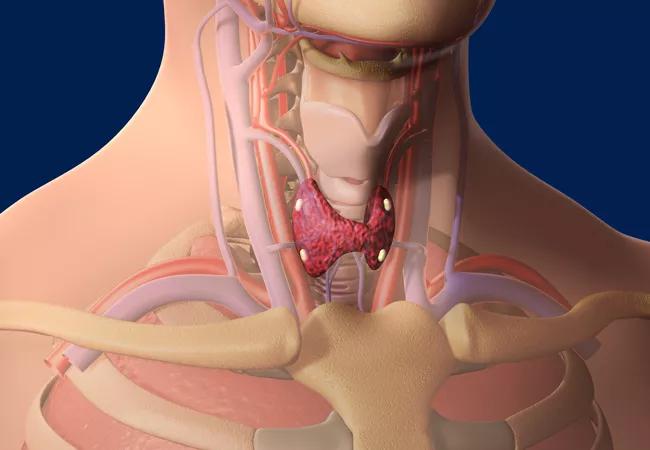
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e5982f51-d198-477d-aa18-4c6dac5c2709/thyroid_650x450_jpg)
thyroid_650x450
A 73-year-old patient presented with fatigue, headaches, disrupted sleep, depression, irritability and extreme thirst. Lab tests indicated hypercalcemia. The patient was referred to endocrinology and diagnosed with hyperparathyroidism. She then met with Cleveland Clinic endocrine surgeon Vikram Krishnamurthy, MD, who used ultrasound to identify an adenoma on one of her four parathyroid glands.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The patient was evaluated for parathyroidectomy, which she had a few weeks later. Following the one-hour procedure, the patient returned home the next morning and reported immediate improvement in her mood and energy level. Subsequent blood tests showed normal calcium levels.
Hyperparathyroidism is the third most common endocrine condition, following diabetes and thyroid disorders. Parathyroidectomy is the predominant treatment for hyperparathyroidism, increasingly performed by endocrine surgeons — a relatively new specialty developed over the past 10 to 20 years.
Dr. Krishnamurthy explains more about the specialty, parathyroidectomy and how it can help patients.
Dr. Krishnamurthy: The current recommendation by experts is that most patients with primary hyperparathyroidism are candidates for parathyroidectomy, provided that there is no contraindication to surgery. Parathyroidectomy is the only way to cure hyperparathyroidism. In experienced hands, that cure rate after surgery is greater than 95 percent. Because parathyroidectomy is minimally invasive, it puts minimal physiologic stress on the body and can be safe even for frail or elderly patients.
Dr. Krishnamurthy: Most patients just require a panel of bloodwork and imaging. The first step is to establish the diagnosis of primary hyperparathyroidism by laboratory testing. In some cases, the diagnosis can be tricky. For these patients, endocrine surgeons and medical endocrinologists in our Parathyroid and Parathyroid Surgery Center work closely to reach a consensus.
Advertisement
After being diagnosed with hyperparathyroidism, patients meet with the surgeon to discuss parathyroidectomy. Before parathyroidectomy, most surgeons will order an ultrasound and a parathyroid scan. All patients should have an ultrasound before surgery to also look for problems with the thyroid, which are common. During consultation, our patients can undergo laboratory testing, parathyroid scan and ultrasound by an endocrine surgeon on the same day.
Dr. Krishnamurthy: The procedure takes 30 to 60 minutes and is done through a single 3-4 cm incision in the patient’s neck. The incision is closed with surgical-grade glue — no staples, stitches or drain. Patients stay for an observation period and are discharged the next morning. Most patients can manage any post-surgery pain with over-the-counter pain relievers.
Dr. Krishnamurthy: After successful surgery, no long-term care is needed. However, patients who developed some degree of bone loss from their primary hyperparathyroidism will likely benefit from taking a daily calcium supplement.
Dr. Krishnamurthy: Numerous studies show that patients experience better outcomes — specifically higher cure rates — if their surgery is performed by a high-volume surgeon. In addition, recent data supports that patients who undergo parathyroidectomy by high-volume surgeons experience statistically significantly:
Patients should feel empowered to ask the surgeon how many parathyroid surgeries they perform each week, month and/or year. High-volume surgeons, particularly those specialty trained in endocrine surgery, have expertise in the most complex parathyroid conditions, including reoperations.
Advertisement
The Department of Endocrine Surgery at Cleveland Clinic is the highest-volume, specialized endocrine surgery center in Ohio, and one of the busiest in the nation. Cleveland Clinic endocrine surgeons perform approximately 1,100 thyroid, parathyroid, adrenal and neuroendocrine surgeries a year — approximately 400 parathyroid surgeries alone.
Advertisement
Advertisement
Pheochromocytoma case underscores the value in considering atypical presentations
Advocacy group underscores need for multidisciplinary expertise
A reconcilable divorce
A review of the latest evidence about purported side effects
High-volume surgery center can make a difference
Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D
Patients spent less time in the hospital and no tumors were missed
A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications