Insulin use at time of hospital discharge can offer clues for the future
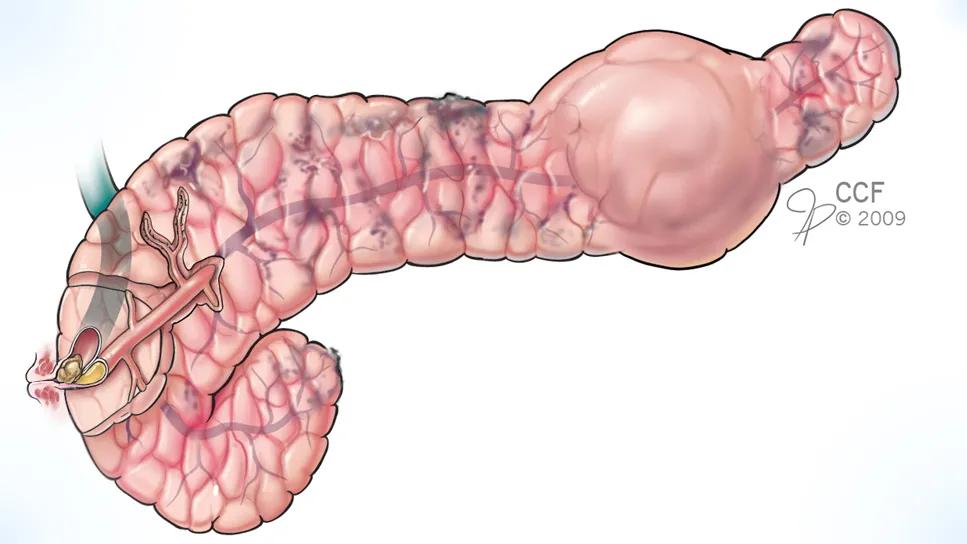
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/63b36993-6366-4f63-99ad-054b9f5ba74e/chronic-pancreatits-study)
medical drawing of a pancreas with pancreatitis
A recent Cleveland Clinic study sheds light on early indicators about whether people with chronic pancreatitis can achieve insulin-independence after undergoing total pancreatectomy with islet cell autotransplantation (TPIAT), a last resort for individuals with severe pain and other symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The research, published in Endocrine Practice (Vol. 30, Issue 8, 752-757), aimed to fill in gaps in the understanding of immediate postoperative predictors of achieving insulin independence within a year after surgery and long term. Its findings can lead to more informed conversations with patients about what they can expect post-surgery, says Keren Zhou, MD, of Cleveland Clinic’s Department of Endocrinology and Metabolism.
“As providers, our impetus was really to better understand how we can more accurately counsel patients immediately following their procedure,” Dr. Zhou says. “We want to understand the early predictors that somebody maybe isn't doing well from a glucose management standpoint and will require long-term medication for treatment of diabetes.”
Chronic pancreatitis often results in severe abdominal pain and gastrointestinal symptoms and can cause fibrosis and serious complications, including diabetes and nutritional malabsorption. TPIAT may be offered when other treatments have failed. Cleveland Clinic has been performing TPIAT for almost 20 years, says Dr. Zhou.
“These are individuals with recurrent hospital admissions,” she says. “Often, they describe feeling like they're not living a life, because they’re always in the hospital, and when not in hospital in chronic pain. It's common to see individuals in their twenties through forties show up for this procedure as their life has been significantly impaired by the pancreatitis.”
The surgery involves removal of the pancreas and isolating insulin-producing islet cells, which are then infused via the splenic vein into the patient’s liver. The procedure is complex and but can be highly successful in eliminating pain. The tradeoff, however, is the risk for diabetes long-term. While some patients who undergo TPIAT have pre-diabetes or diabetes before the surgery, most do not, so this would be a new diagnosis post-surgery.
Advertisement
“For these individuals, having this procedure puts them at risk of needing some form of medication for pancreatic diabetes. They literally can go from no dysglycemia to immediate pancreatic diabetes,” she says.
The researchers conducted a retrospective review of Cleveland Clinic patients who received TPIAT between January 2010 and December 2022, were 18 or older and had a confirmed chronic pancreatitis diagnosis. The average length of time between diagnosis and surgery was 77.5 months.
Of the 46 patients included in the final analysis, 29 (63%) had preoperative HbA1c of 5.7% or higher.
The study identified several key factors associated with whether a patient will need to go on insulin after the surgery, including:
“We saw that even having lower units of basal insulin at the time of discharge from the hospital was significantly associated with being insulin-free in the short run and also in the long run,” says Dr. Zhou. “At one-plus years out from the procedure, every additional unit of insulin that the patient was on at the time of discharge was associated with a 32% decrease in the likelihood of long-term insulin independence.”
Advertisement
“We also found that our overall rates of insulin independence were not very good,” she adds. “Seven of 46 patients (15.2%) who had long-term follow-up data were able to maintain insulin independence at their most recent follow-up. Traditional counseling for this procedure has suggested that a third of individuals will end up on insulin, a third will have a minimal medication requirement and third will be insulin free and diabetes free. Unfortunately, this does not seem to be the case long-term.”
This data puts clinicians in a better position, at the time of discharge, to identify individuals who are more likely to be insulin dependent in the short and long run, Dr. Zhou says.
“If a patient comes back in a month and asks how likely it is they will come off insulin," she says, "we can use some of these additional pieces of information to make an assessment of the likelihood for insulin independence. Then we can start talking about advanced diabetes management such as an insulin pump when insulin independence seems unlikely.”
Advertisement
Advertisement
Pancreas and spleen removed to minimize risk of pancreatic cancer
Pheochromocytoma case underscores the value in considering atypical presentations
Advocacy group underscores need for multidisciplinary expertise
A reconcilable divorce
A review of the latest evidence about purported side effects
High-volume surgery center can make a difference
Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D
Patients spent less time in the hospital and no tumors were missed