Analysis examines surgical resection of rare pituitary tumors
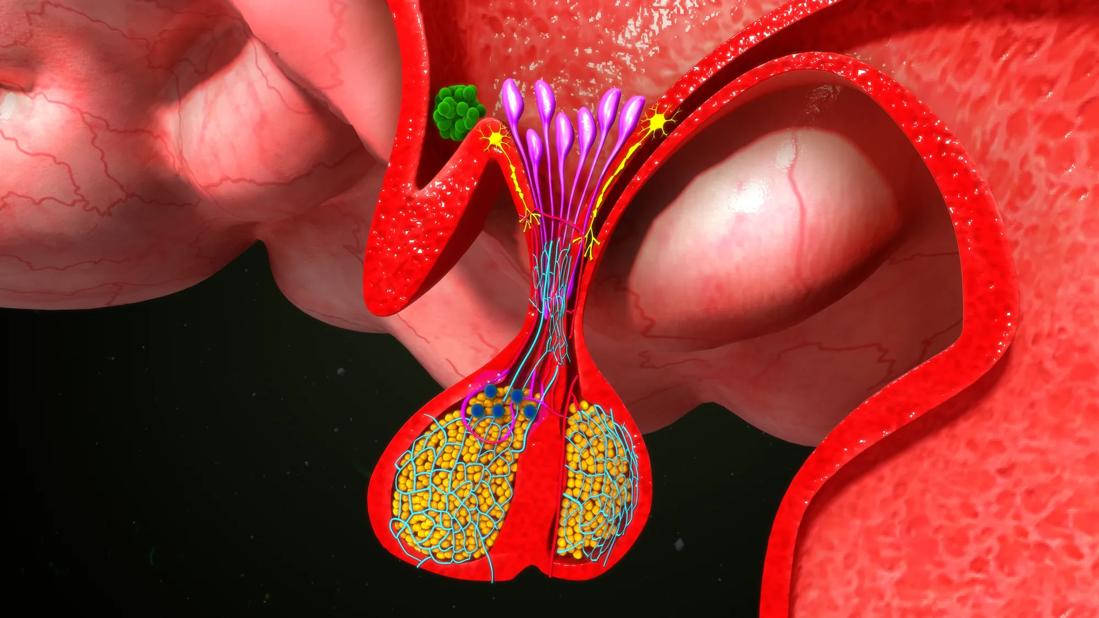
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/562ca54a-a9cb-4e4a-9798-5d90ffae65f3/pituitary-609698908)
Pituitary gland
Prolactinomas are the most common type of pituitary tumor, and the vast majority measure a few centimeters wide. When the tumor exceeds 4 cm, it’s considered a giant prolactinoma (GP).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“These are very rare tumors that can masquerade as other types of brain tumors and not get the specific attention they deserve,” says Divya Yogi-Morren, MD, medical director of Cleveland Clinic’s Pituitary Center. “It’s very important that we are aware of how they present and that we monitor prolactin levels.”
Medical therapy with dopamine agonists is the first-line treatment for prolactinomas, including GPs. Surgical intervention is required in 13% to 14% of GP cases.
“There is a paucity of data surrounding second-line management of giant prolactinomas with surgery,” says Dr. Yogi-Morren. She collaborated with colleagues from the Pituitary Center on a descriptive study of surgical management of giant prolactinomas and published results in the International Journal of Endocrinology.
The team conducted a retrospective analysis of patients who underwent surgery for functional prolactinomas at Cleveland Clinic from 2003 to 2018. There were 79 total patients, eight of whom (10%) had benign GP and were included in the study. The tumors ranged from 4.6 to 7.7 cm, with a median dimension of 6 cm.
“These are large tumors that occupy a lot of space and cause problems,” says Dr. Yogi-Morren. “All of the patients in our study presented with mass effects, which means they were causing pressure on the structures around the tumor.”
These included:
Six patients received dopamine agonist therapy before surgery. None of the surgical resections were complete, and all the patients received postoperative medical treatment.
Advertisement
The patients were followed for a median of 5.5 years. None achieved remission off of dopamine agonist (DA) therapy, but 63% reached remission while on ongoing DA therapy at the median time of three years after initial surgery.
“Prior to surgery, these tumors were so large that they were overcoming any effect from the medication,” says Dr. Yogi-Morren. “Debulking of the tumor through surgical resection allows for a better response to medication.”
While medication remains the frontline therapy for prolactinomas, surgical management should be considered on a case-by-case basis.
“The success rate of medical treatment is approximately 70% to 80% for macroprolactinomas that respond to dopamine agonists alone,” says Dr. Yogi-Morren. “But if your patient happens to be in the 20% to 30% that did not respond to medication, that is an indication for surgery.”
Other candidates for surgery are patients who can’t tolerate the medication.
“This is something we see fairly frequently. We start the medication, and they have dizziness, headaches and are some have severe side effects that affect mobility and the ability to carry about the activities of daily living,” says Dr. Yogi-Morren.
She adds that patient choice should also be considered.
“It’s our responsibility to give them all the viable options,” says Dr. Yogi-Morren. “I always ask patients, ‘Tell me what kind of person you are. If you know there is a lump or bump in your body, do you just want it out? Or are you the kind of person who is content to monitor it?’”
Advertisement
Dr. Yogi-Morren encourages endocrinologists to educate patients with GPs about surgical options and to set expectations about outcomes and potential side effects, such as hypopituitarism. Then, if patients are good candidates for surgical management, refer them to a center of excellence that has dedicated pituitary surgeons.
“We shouldn’t be afraid to use every single tool we have to manage giant prolactinomas, and one of those tools is surgery,” says Dr. Yogi-Morren. “Go ahead and hit it hard with everything you have, then the patient might have a better response to medication and radiation afterward.”
Advertisement
Advertisement
A range of pituitary tumor-related conditions all benefit from a multidisciplinary approach
Giving young patients a hand as they take charge of their own health
Case illustrates how easily condition can mimic preeclampsia
Cleveland Clinic endocrinologists work to identify protocols for improving care
Building the bridge between endocrinology and geriatrics
ACC committee underscores need to properly weigh benefits in risk-benefit calculations
Randomized controlled trial finds no quality-of-life benefit after standard pituitary tumor surgery
Pheochromocytoma case underscores the value in considering atypical presentations