Radiofrequency ablation significantly reduces symptom severity, shrinks nodules

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3b69dfb5-8e6f-4ad1-b9b7-100ecb19850b/ablation-surgery)
Ablation surgery image
Radiofrequency ablation (RFA) has gained traction in the U.S. in recent years as a safe and effective alternative to lobectomy or thyroidectomy to treat selected benign thyroid nodules. Success, however, has been measured primarily by reduction in tumor size.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A recent study by Cleveland Clinic specialists who perform RFA for thyroid nodules presents additional insights into symptom improvement thanks to a validated assessment tool that compares patient-reported symptoms before RFA and at again at two weeks, three months and six months post-treatment.
The results: Significant symptom reduction was detected at three and six months after thyroid RFA using an objective patient symptom questionnaire.
“In addition to demonstrating that the nodules shrank, we also showed that the patients’ symptoms really decreased in severity,” says Eren Berber, MD, MBA, a Cleveland Clinic endocrine surgeon, who is the director of the program and performed the procedures. “Their symptom scores, which were elevated before the ablation, decreased over time.”
Because nodules can cause patients significant discomfort and distress about changes in their appearance, it is important to incorporate reliable patient-reported data in the ongoing assessment of the use of RFA as an alternative to traditional surgery.
Although benign thyroid nodules are common, and the majority cause no symptoms, about 15% of individuals experience discomfort.
“When nodules reach a certain size, or when they're in certain locations, patients can experience pressure in their neck, difficulty swallowing and difficulty breathing,” Dr. Berber says. “They also might feel some discomfort if they turn their head a certain way. Sometimes the patient assumes this is normal, but it isn’t.”
Traditional surgery to remove the thyroid gland prevailingly succeeds, but the surgery carries downsides such as recovery time, scarring and a lifelong need for thyroid medication. “If you remove only half of the thyroid, which is the smallest operation we do, the likelihood of the patient requiring the thyroid pill is about 50%.”
Advertisement
Introduced in South Korea in 2006, RFA for thyroid nodules has earned a reputation as a safe and effective alternative to conventional surgery. In the United States, the procedure has become more fully embraced over the last two years as RFA needles have become available that are tailored for the precision required when performing ablation around the thyroid.
RFA for thyroid nodules is appropriate only for patients who have had two biopsies confirming the nodules are benign. The procedure is currently not recommended for treating thyroid cancer. RFA also may be contraindicated for nodules located too close to the airway, laryngeal nerve, major arteries or esophagus.
The surgery is performed under local anesthesia in an operating room using an ultrasound probe for guidance and thyroid-specific RFA probes in varying sizes of the active tip (5 mm, 7 mm or 10mm), depending on nodule size. Ablation should begin near the deep part of the nodule and be gradually moved back, as bubbles appear, until the whole nodule is ablated except for margins near critical structures. Once ablation is complete, pressure is applied for 10 minutes to the thyroid and the skin is bandaged. The patient is observed for two hours before discharge. There are no restrictions after the procedure.
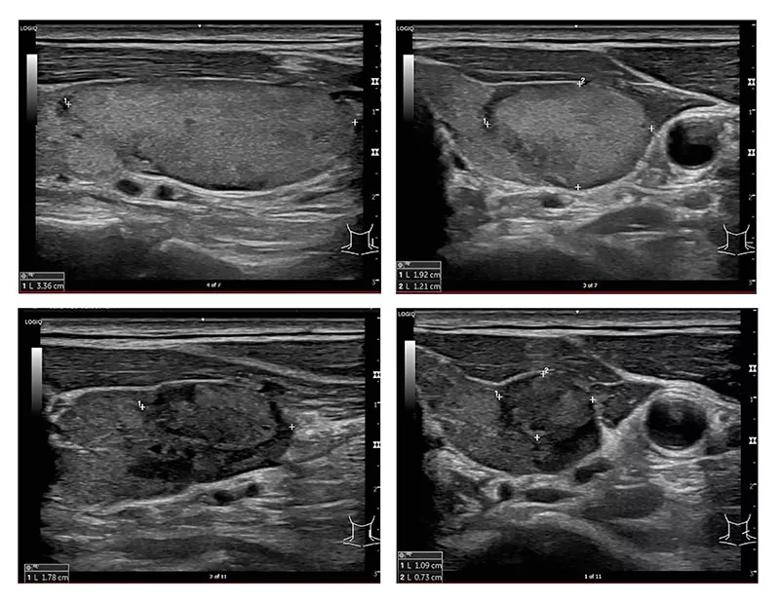
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d9706f5a-6297-4436-9f5c-88eebc526805/treated-thyroid-nodules)
Clockwise from top left, these images show the decrease in nodule size over time, from 4 cubic centimeters before RFA to 0.7 cubic centimeters at six months post-treatment.
In 2022, Cleveland Clinic performed a prospective study of RFA for thyroid nodules and measured symptom relief using patient-reported outcome measures. Twenty-five patients who underwent the procedure were evaluated at baseline, two weeks, three months and six months with the Patient-Reported Outcomes Measurement for Parathyroid and Thyroid Disease (PROMPT). Thyroid ultrasound and complications were evaluated at the same intervals.
Advertisement
PROMPT uses 30 questions and a zero-to-100 scale to assess symptoms related to cervical compression from thyroid nodules and symptoms that might be attributable to hyperparathyroidism. The tool has been validated for evaluating symptom improvement after thyroidectomy.
During the study, 25 patients (84% female; mean age 51 years) underwent radiofrequency ablation, and 32 nodules were treated. The baseline mean nodule volume and largest dimension were 13 ± 11 mL and 3.4 ± 1 cm, respectively. Significant changes in PROMPT comprehensive scores were seen at three months (38.9 ± 26.4 to 21.0 ± 21.4; P ¼.004) and six months (32.7 ± 19.9 to 17.5 ± 21.0; P ¼.02) but not at two weeks (41.0 ± 22.7 to 36.1 ± 21.9; P ¼ .28). Significant volume and size reductions were seen at all three post-treatment points. Two complications occurred.
The data is important because the efficacy of any innovative technology should we verified using objective parameters, says Dr. Berber.
“It is important to show that patients get benefits that are similar to other treatment avenues,” he says. “We wanted to make sure that we were not biased and that the patients were not biased. When we looked in the literature, we found no other study that applied such an objective and comprehensive validated scale.”
While the use of RFA for thyroid nodules has become more common, Dr. Berber emphasizes that it’s important for the procedure to be done in the proper setting by experienced teams. Cleveland Clinic has performed about 60 of these procedures since 2022.
Advertisement
“This procedure requires significant expertise in conventional surgery, ultrasound and ultrasound-guided procedures. The procedures currently are done in the operating room in order to maintain the safety of the patients,” says Dr. Berber. “We are ready to do thyroid surgery for complications like bleeding or rupture, although we haven’t seen any.”
“At Cleveland Clinic, we have a big experience with conventional surgery, ultrasound and ultrasound-guided procedures,” he adds. “We also have a lot of experience with ablation of other organs, such as the liver, adrenal glands other solid organs. For patient safety and success, it’s important to join all these skills.”
Advertisement
Advertisement
Add AI to the list of tools expected to advance care for pain patients
Telehealth aids in treatment of fibromyalgia and median arcuate ligament syndrome
Program enhances cooperation between traditional and non-pharmacologic care
A surgeon’s perspective: three patient groups
Compassion, communication and critical thinking are key
Cleveland Clinic study investigated standard regimen
Despite the condition’s debilitating, electric shock-like pain, treatment options are better than ever
Program participation correlates with reduced use of opioids, X-rays and ED visits