When conservative approaches don’t work, it may be time to turn to sacroplasty
A 51-year-old patient with breast cancer was referred to Cleveland Clinic’s Department of Pain Management for pelvic pain refractory to fentanyl patches, gabapentin and venlafaxine. She had been diagnosed with breast cancer in 2008, had a mastectomy in 2009 and was treated with chemotherapy. She began palliative radiation therapy in 2018 due to multiple metastases to her spine and pelvis. She also underwent surgery for osteonecrosis in her right jaw. Kyle Neale, DO, staff in Cleveland Clinic Cancer Center’s Department of Palliative & Supportive Care, referred her to Sherif Costandi, MD, an interventional pain management specialist when other measures failed.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
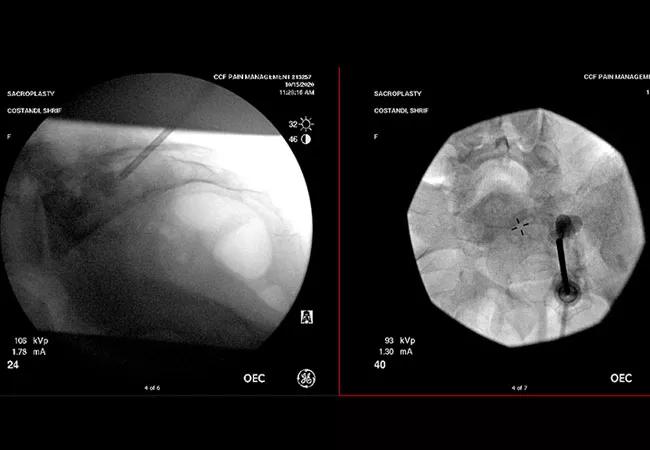
Magnetic resonance imaging (MRI) of the pelvis in June 2020 showed pathologic sacral fractures. Because the patient failed palliative medications and radiotherapy, Dr. Costandi performed a percutaneous sacroplasty under deep sedation. Guided by fluoroscopy, he accessed the sacral bone and delivered polymethylmethacrylate known as bone cement, carefully avoiding the nerve roots in the sacral foramen.
The patient recovered well. Upon follow-up, the patient reported that her pain had dropped from 8/10 to 2/10.
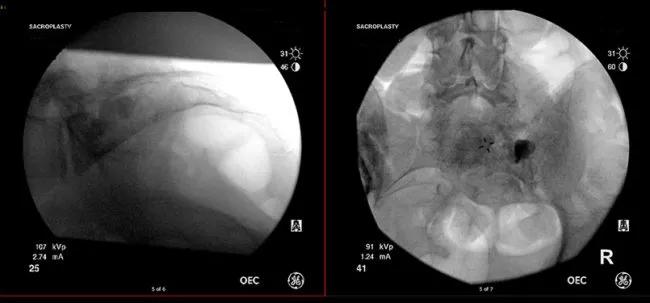
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4dfe28bb-8732-4408-a535-2c0965126699/r-and-lateral-images-after-injection-of-cement-and-pulling-out-the-instruments_805x375-650x303-1_jpg)
Antero-posterior and lateral images after injection of cement and pulling out the instruments. Above: Antero-posterior and lateral images of sacroplasty technique.
Some of the sacral fractures are pathological as a result of a cancerous process. Furthermore, a number of cancer pain patients are exposed to radiation, and a small group of them may develop sacral fractures from radiation. Because cancer and radiation weaken your bones, it can be very challenging for them to heal on their own. Those patients might benefit from sacroplasty. For patients who have cancer, sacroplasty has the potential to relieve the pain and stabilize the broken segments or the broken sacrum,” says Dr. Costandi.
Other patients who could be good candidates for sacroplasty are those who have developed sacral fractures from traumatic events, such as a fall or car accidents, but have not responded well to regular or conservative measures. Most sacral fractures heal within weeks, but there’s a small portion of them that don’t heal. For these patients, sacroplasty might provide pain relief.
Advertisement
Although the number of physicians who perform sacroplasties is small, the technique is very safe in the hands of trained physicians, says Dr. Costandi. There are specific measures that are taken to ensure patient safety, including imaging guidance. This is used to direct the needle and properly inject the cement to ensure there is not any leakage.
Dr. Costandi was drawn to sacroplasty because of a desire to help and treat pain in his cancer patients. “I’ve had patients with sacral cancer metastases that had cancer that has destroyed their bones, and they’ve developed microfractures there. Microfractures greatly affect mobility and become an incredible burden because of how painful it is to take steps.” Sacroplasty provides patient with significant and fast relief that positively help the patient to regain their desired quality of life.
Advertisement
Advertisement

Researchers seek solutions to siloed care, missed diagnoses and limited access to trauma-informed therapies

Study participants also reported better sleep quality and reduced use of pain medications

Two-hour training helps patients expand skills that return a sense of control

Program enhances cooperation between traditional and non-pharmacologic care

National Institutes of Health grant supports Cleveland Clinic study of first mechanism-guided therapy for CRPS

Pain specialists can play a role in identifying surgical candidates

Individual needs should be matched to technological features

New technologies and tools offer hope for fuller understanding