Study shows that intravitreal injections may significantly slow the disease once thought untreatable
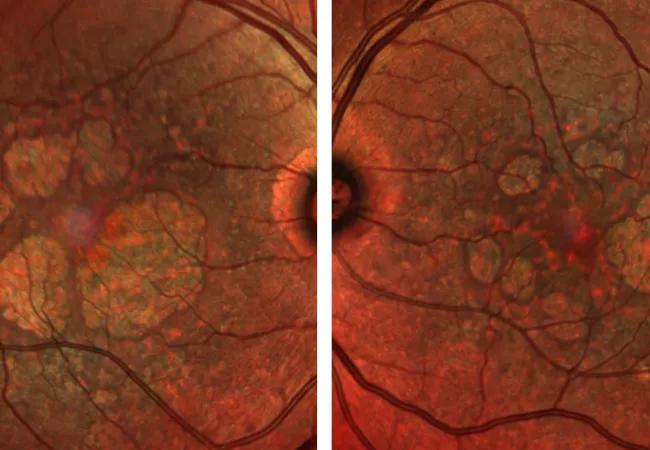
There is currently no treatment for geographic atrophy — the “dry” form of macular degeneration, a leading cause of blindness in the U.S. and worldwide. Now a new study has shown that the drug pegcetacoplan can significantly slow the disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Two phase 3 clinical trials showed that injecting pegcetacoplan monthly and every other month resulted in a significant reduction in lesion growth. The study also found that pegcetacoplan was generally safe and well tolerated, although a small number of patients converted to “wet” macular degeneration, which is treatable.
“This is a first step in treating this debilitating disease,” says ophthalmologist and retina specialist Rishi P. Singh, MD, of Cleveland Clinic’s Cole Eye Institute. “It represents a breakthrough therapy for patients with this condition and potentially could reduce legal blindness around the world.”
Dr. Singh presented the top-line findings from the phase 3 study at the American Academy of Ophthalmology 2021 meeting.
The study built on previous research that showed that dry macular degeneration is linked to the complement system and a hyperactive immune response that damages the eyes. Pegcetacoplan is a complement system inhibitor that has previously been used to treat paroxysmal nocturnal hemoglobinuria, a rare autoimmune disorder linked to a systemic complement cascade.
The study involved two multicenter, phase 3 clinical trials (DERBY and OAKS) involving a total of more than 1,250 patients with geographic atrophy. Patients were randomized to receive injections of 15 mg of pegcetacoplan monthly or every other month, or a sham injection monthly or every other month.
In the combined results of the two trials, patients who received the drug monthly showed a 17% reduction in geographic atrophy lesions after 12 months, compared to those who received sham injections, while those who were injected every other month had a 14% reduction.
Advertisement
Patients with extrafoveal lesions had an even stronger response, with a 26% reduction in lesions with monthly injections and 23% reduction with every-other-month injections compared to the sham group.
“We expected this drug to work, but it exceeded my expectations,” says Dr. Singh.
The drug was generally safe and well-tolerated. The most common side effects were conjunctival hemorrhage, eye pain and vitreous floaters.
However, around 7% of patients developed wet macular degeneration as a result of the medication, not as a normal progression of the disease.
“That’s definitely a concern,” says Dr. Singh. “While this is breakthrough therapy, the conversions to wet macular degeneration are noteworthy for clinicians and patients.”
Wet macular degeneration can be treated with currently available anti-VEGF agents, he notes.
Results of the study are planned to be submitted to the FDA for review by the end of 2021, with a decision on FDA approval for clinical use anticipated in early 2022.
Dr. Singh said the findings are a significant step forward in the treatment of macular degeneration, which affects an estimated 1 million people in the U.S.
“For years we’ve been telling ophthalmologists and patients that there’s no treatment for this condition — that it’s just a matter of aging, that its progression is inevitable over time and that there’s nothing we can do,” he says. “Finally, this drug can show a reduced progression of the disease if given monthly or every other month. It’s a game changer.”
Advertisement
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift