Pediatric heart failure and transplant cardiologist discusses his research approach

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
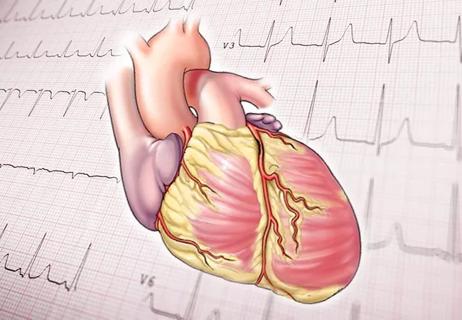
As a clinician caring for children with heart failure, it is disheartening that the science of pediatric heart failure has not advanced and accelerated at a rate comparable with adult heart failure. There are numerous large-scale adult heart failure studies that have researched epidemiology and, subsequently, risk factors, outcomes, and therapies to improve outcomes for these patients.
Unfortunately, large-scale epidemiological studies are lacking in the field of pediatric heart failure. These epidemiological studies are an important first step to understanding the burden of this deadly disease before we can develop measures to treat it. A monumental methodological challenge for me was “How do we capture the true burden of this illness in a comprehensive manner?”
To conduct this important analysis, I sought the expertise of Cleveland Clinic’s Center for Population Health Research. They helped me tremendously by designing the study and conducting rigorous statistical analyses required to complete such a large-scale epidemiological study.
We had a few important aims: A. Describe the burden of heart failure (both primary and comorbid) across the U.S. healthcare system (in the emergency department, in-hospital admissions, and mortality) in 2012 and 2016. B. Highlight inpatient costs for pediatric patients admitted with heart failure, and C. Compare the burden, resource use, and outcomes for children to adults with heart failure.
To do so, we utilized four national registries that captured patients of all ages and insurance statuses with and without heart failure across the U.S. healthcare system in 2012 and 2016.
Advertisement
Our study had several novel and important findings: First, we found that the overall burden of pediatric heart failure is rising. Compared to adults, children with heart failure who came to the emergency department or were hospitalized were at an increased risk for mortality, need for advanced cardiac therapies, such as extracorporeal membrane oxygenation, ventricular assist device and heart transplant, and required increased utilization of resources.
We found that the top three indications for heart failure-related emergency department visits and hospitalizations among children were congenital heart disease, cardiomyopathy, and conduction disorders/arrhythmias.
Finally, children with heart failure had two-fold increased emergency department charges and a 24-fold increased hospitalization charges than children without heart failure, highlighting the burden this illness places on the U.S. healthcare system.
We evaluated records across the U.S. healthcare system to identify children with and without heart failure and then compared this to health records for adults with heart failure. To my knowledge, such an extensive analysis has never been conducted before in pediatrics. It took us over two years to get this study from inception to publication and required tremendous coordination and collaboration with the statistical team at the Center for Population Health Research.
We are currently conducting additional population health studies to further bridge important knowledge gaps in the field of pediatric heart failure and heart transplant.
Advertisement
About the author: Dr. Amdani is a pediatric cardiomyopathy, heart failure and transplant physician in the Department of Pediatric Cardiology and Assistant Professor of Pediatrics, Cleveland Clinic Lerner College of Medicine at Case Western Reserve University.
Advertisement
Advertisement

Experts are challenging the one-size-fits-all paradigm

Decongestion, therapy titration and readmission rates comparable to those with traditional hospital care

Panel proposes staging and treatment protocols that support harmonized evaluation and management of heart failure in patients with congenital heart disease

Eminent clinician-researcher brings special expertise in nutritional interventions for heart failure

Recent volume and outcomes data in two major realms of cardiovascular care

Volatile organic compounds have potential in heart failure diagnostics

Basic understanding of condition and treatment is lacking
Indications and issues concerning cardiac resynchronization therapy, conduction system pacing