Findings from more than 7,500 donor-recipient pairs
In the field of heart transplantation, the conventional method for determining donor-recipient (D-R) size matching has been using height and weight assessment. However, total cardiac volume (TCV) may be the optimal tool for predicting graft survival, according to the findings from a recent study published in JACC: Heart Failure. Adopting a standardized approach to size matching across centers could be key to reducing donor heart discard and ultimately allow more children with end-stage heart failure to get transplanted.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pediatric transplant cardiologist Shahnawaz Amdani, MD, first author of the study, says the D-R heart match is a critical consideration every time a center accepts a donor heart for a patient who needs a transplant. “The first thing we look at is how the donor’s heart matches with the recipient’s heart. Until recently, the only way to determine a match was to make an educated guess based on the donor and recipient’s height and weight.”
It’s a decision that needs to be made decisively and, occasionally, at an unexpected hour—like in the middle of the night—making accuracy and simplicity of these metrics essential.
The traditional inputs of height and weight have been a reliable metric for D-R matching since the beginning of heart transplantation. These variables are also collected by United Network for Organ Sharing (UNOS). The impetus for rethinking this assumption, explains Dr. Amdani, is twofold: increasing rates of obesity and emerging imaging technology.
The rates of obesity have increased significantly in both general and pediatric populations, calling the presumed accuracy of these metrics into question. For example, a younger child with a similar weight to that of a much older child may appear on paper to be an appropriate match, but the “true heart size discrepancy” could put them at risk for suboptimal posttransplant outcomes.
Unlike adults where predicted heart mass has emerged as a metric accepted by all adult heart transplant cardiologists for D-R matching, to date, there is no such universally accepted metric for pediatric heart transplant candidates.
Advertisement
Dr. Amdani recalls discourse following a 2019 International Society for Heart and Lung Transplantation pediatric report, for which the theme was D-R size matching. It was suggested that weight may be the best measure for D-R matching in pediatric heart transplant, an assumption that led Dr. Amdani and team on a quest for answers.
Using the Pediatric Heart Transplant Society database, the team analyzed data from 7,715 D-R pairs over the span of nearly two decades (1993-2021). Their primary aim was to determine metrics of size mismatch that could predict graft survival at one and five years posttransplant. Specifically, they examined the effects of size mismatch by height, weight, body mass index, body surface area, predicted heart mass and TCV on graft survival, rejection, and cardiac allograft vasculopathy.1
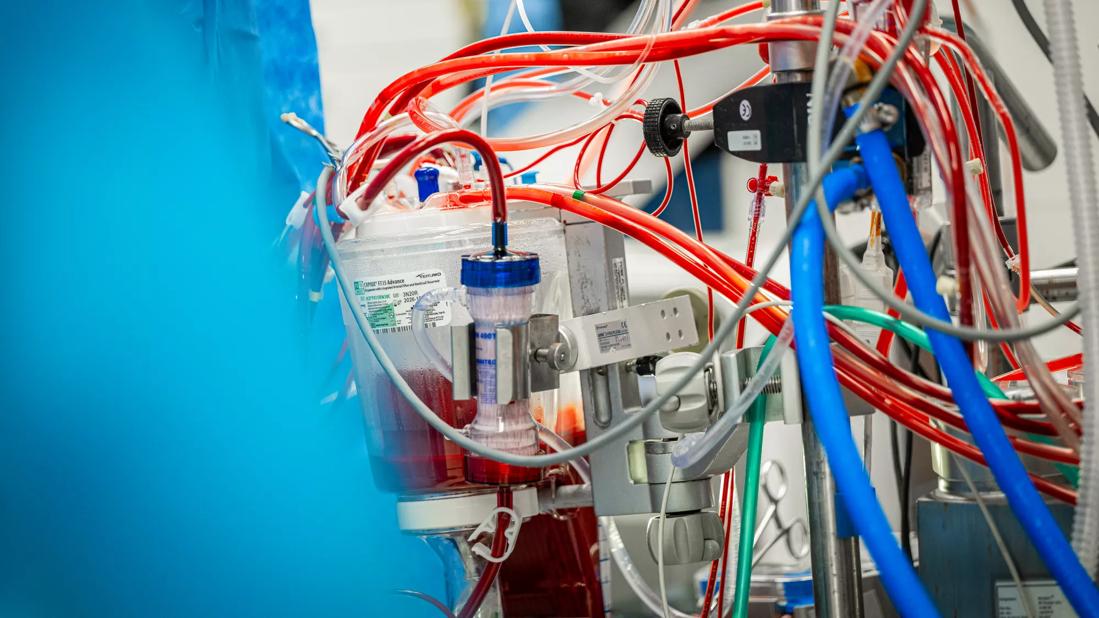
Because the newer models, PHM and TCV, rely on advanced cardiac imaging data (CT, MRI), and these were not available to the study team, the team instead used validated formulas to calculate D-R predicted heart mass and total cardiac volume.
Notably, their findings revealed a wide discrepancy of D-R mismatch depending on the variable that was used. Only 36% of pairs were well-matched using the weight metric alone, while height and TCV metrics provided a much higher predictive match rate at 71% and 93%, respectively.
Other findings about height and estimated TCV metrics in posttransplant graft survival are as follows.
Advertisement
These findings raise an important point about looking at TCV more prospectively to understand and refine parameters for accepting a donor heart based on this metric, which holds great potential but is currently underexplored.
While many experts, like Dr. Amdani, favor use of the TCV metric, its broader adoption within the pediatric heart transplant community will require seamless integration into practice, something he says is still not yet available for practical use.
“To integrate TCV-based matching into clinical practice, we need some sophistication as to how the volumes are calculated and, subsequently, D-R pairs matched. As a clinician, I should be able to input minimal amount of data and have a calculator that accurately demonstrates how matched the donor cardiac volume is relative to the recipient’s cardiac volume,” he says.
But it’s time we rethink our assumptions about traditional height and weight approaches that have been around for 30-plus years and may not be the best ways to match donor-recipient hearts in 2023.”
Reference
Advertisement
Advertisement

Largest study to date confirms mortality rates similar to DBD transplant and reveals risk factors

More than 30% of patients die when early dialysis is needed after surgery

Highlights and insights from recent Cleveland Clinic experience

Results from a large registry study provide an updated picture of recurrent rejection
Study validates a noninvasive alternative to invasive coronary angiography

Multimodal evaluations reveal more anatomic details to inform treatment

A closer look at the impact on procedures and patient outcomes

Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve