Category debug info: client: {"assets":{},"datasets":{},"live":{},"projects":{},"users":{},"observable":{"assets":{},"datasets":{},"live":{},"projects":{},"users":{}}} Now: 1770640393035 Cache Key: cqdDataBySlug:primary-care fetchCache[cqdDataBySlug:primary-care].expirationTime: falsey fetchCache[cqdDataBySlug:primary-care]. seconds remaining: falsey All fetchCache expiration times: -- Key: cqdNotFoundPage, seconds remaining: 7827 -- Key: cqdDataBySlug:postoperative-acute-kidney-injury-following-fontan-conversion-surgery-understanding-risk-and-managing-care, seconds remaining: -14309 -- Key: cqdDataBySlug:a-new-era-of-management-for-diabetic-kidney-disease, seconds remaining: -12314 -- Key: cqdDataBySlug:clinical-cardiology, seconds remaining: -11001 -- Key: cqdPostsByCategory:cqd-migrated-category-22925,1,10, seconds remaining: -10227 -- Key: cqdDataBySlug:coaching-parents-on-the-importance-of-practicing-social-skills-in-nontherapeutic-situations, seconds remaining: -10659 -- Key: cqdDataBySlug:collaboration-between-acute-care-and-rehab-hospitals-drives-down-readmissions-in-stroke-patients, seconds remaining: -9961 -- Key: cqdDataBySlug:mri-may-be-best-tool-for-tumor-staging-and-detecting-bilateral-disease-in-invasive-lobular-carcinoma, seconds remaining: -9783 -- Key: cqdDataBySlug:why-lead-safety-has-become-cleveland-clinics-top-priority-for-community-health, seconds remaining: -9488 -- Key: cqdDataBySlug:getting-a-good-nights-sleep-the-importance-of-sleep-hygiene-podcast, seconds remaining: -6165 -- Key: cqdDataBySlug:epstein-barr-virus-serologic-screening-for-nasopharyngeal-carcinoma-is-cost-effective-in-southern-china, seconds remaining: -6348 -- Key: cqdDataBySlug:leading-nurses-in-a-new-era-of-healthcare, seconds remaining: -5807 -- Key: cqdDataBySlug:research-rheumatology-immunology, seconds remaining: -5413 -- Key: cqdPostsByCategory:cqd-migrated-category-2624,1,10, seconds remaining: -4851 -- Key: cqdDataBySlug:asymptomatic-aortic-dissection-after-orthotopic-heart-transplantation-in-a-pediatric-patient, seconds remaining: -4904 -- Key: cqdDataBySlug:innovative-approaches-in-pediatric-hepatology-help-patients-live-with-the-liver-they-have, seconds remaining: -4174 -- Key: cqdDataBySlug:news-insight-cancer, seconds remaining: -3270 -- Key: cqdPostsByCategory:cqd-migrated-category-2547,17,10, seconds remaining: -2625 -- Key: cqdDataBySlug:biomarkers-as-predictors-to-suicidal-risk-in-adolescents-a-1-year-follow-up-study, seconds remaining: -2540 -- Key: cqdDataBySlug:the-role-of-hip-resurfacing-in-orthopaedic-care, seconds remaining: -1640 -- Key: cqdDataBySlug:study-sheds-new-light-on-the-role-of-prohibitin-in-wilms-tumor, seconds remaining: 1122 -- Key: cqdDataBySlug:case-study-candid-discussions-illuminate-value-of-simple-pleasures-in-elderly-woman-with-severe-dementia, seconds remaining: 1661 -- Key: cqdDataBySlug:3d-printed-implant-reconstructs-hip-in-patient-with-no-proximal-femur-or-pelvis, seconds remaining: 2056 -- Key: cqdDataBySlug:positive-airway-pressure-therapy-and-covid-19-what-patients-need-to-know, seconds remaining: 2964 -- Key: cqdDataBySlug:glucocorticoid-induced-adrenal-insufficiency-and-glucocorticoid-withdrawal-syndrome, seconds remaining: 3833 -- Key: cqdDataBySlug:patients-will-soon-have-an-additional-option-when-new-osteoporosis-treatment-hits-market, seconds remaining: 3691 -- Key: cqdDataBySlug:how-were-powering-up-innovation-in-the-digestive-disease-surgery-institute, seconds remaining: 4384 -- Key: cqdDataBySlug:cytokine-storm-and-the-prospects-for-immunotherapy-with-covid-19, seconds remaining: 5643 -- Key: cqdDataBySlug:dementia-with-lewy-bodies-consortium-extends-research-efforts-with-10-7m-nih-renewal-grant, seconds remaining: 7999 -- Key: cqdDataBySlug:unravelling-the-mysteries-of-sepsis-and-septic-shock, seconds remaining: 7827 -- Key: cqdDataBySlug:solriamfetol-demonstrates-safety-efficacy-for-wakefulness-in-1-year-extension-trial, seconds remaining: 8211 -- Key: cqdDataBySlug:research-supports-minimally-invasive-surgery-for-older-patients-with-endometrial-cancer, seconds remaining: 8546 -- Key: cqdDataBySlug:innovation-in-facial-reanimation-is-helping-more-patients-smile, seconds remaining: 8932 conditions: -- false, -- NA, -- NA, -- NA -- false Cache miss for key cqdDataBySlug:primary-care - retrieving from Sanity CCCache.dataFetchCount: 9471 Cache cleanup seconds remaining: 5691
Advertisement
Advertisement
Emerging evidence suggests a patient-specific approach
How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians
Cleveland Clinic study investigated standard regimen
Not if they meet at least one criterion for presumptive evidence of immunity
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Essential prescribing tips for patients with sulfonamide allergies
Confounding symptoms and a complex medical history prove diagnostically challenging
For patients with headache, pulsatile tinnitus or vision changes, immediately stop use and refer to ophthalmology
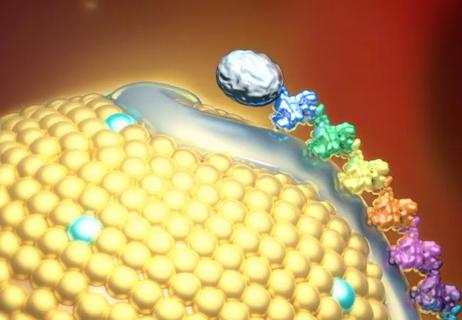
Phase 2 trial of zerlasiran yields first demonstration of longer effect with each dose of an siRNA
Cleveland Clinic’s Esports Medicine team weighs in on importance of multidisciplinary care
Cleveland Clinic Cognitive Battery identifies at-risk patients during Medicare annual visits
Rendered: Mon Feb 09 2026 12:33:13 GMT+0000 (Coordinated Universal Time)
9500 Euclid Avenue, Cleveland, Ohio 44195 |
800.223.2273 | ©
2026 Cleveland Clinic. All Rights Reserved.