OMT may be right for some with Graves’ eye disease

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0e6693cd-c014-4192-bbac-79a16e277e72/Osteopathic-Treatment-with-Grave-s-Ophthalmopathy)
Osteopathic practitioner manipulating patient's face
The photo above illustrates the correct hand contact for eye socket release.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 63-year-old patient had been undergoing successful osteopathic manipulative treatment (OMT) for chronic migraine, neck and back pain when she sought help with new symptoms: eye pressure, swelling and excessive tearing related to Graves’ disease.
Graves' disease is an autoimmune thyroid disorder that affects 1% of Americans, about half of whom develop Graves’ ophthalmopathy (GO). Treatment options vary depending on symptom severity and range from artificial tears (to relieve dryness) to glucocorticoids to surgery.
This patient was receiving IV glucocorticoids, but still had GO symptoms, which can include eyelid retraction, vision loss, exophthalmos (eye protrusion), disfigurement and pain.
In consultation with her doctor, Katrina Rakowsky, DO, Chair of Cleveland Clinic South Pointe Hospital’s Division of Osteopathic Neuromusculoskeletal Medicine, the patient decided to pursue OMT for her eye discomfort. She underwent 16 OMT sessions over two years. While her endocrinologist medically managed her thyroid hormone levels, Dr. Rakowsky addressed biomechanical and circulatory factors affecting the eyes by using manipulative techniques, including:
At virtually every visit, the patient described an immediate reduction of pressure. She experienced no adverse effects, and her treatment continued until her GO stabilized and she was satisfied with her results. Although she still receives OMT for neck pain, she has not reported the return of any GO symptoms in the three years since her treatment.
Advertisement
Dr. Rakowsky hopes that the case, reported in the International Journal of Osteopathic Medicine, will raise awareness of how OMT might serve other patients with GO.
“Structural problems anywhere in the body will affect function anywhere in the body,” says Dr. Rakowsky. “Doctors who treat patients with GO may not be aware of non-surgical, biomechanical and circulatory treatments for symptoms related to structural eye problems. Patients with GO may benefit from a referral to OMT as an additional treatment option. If we can manage a patient’s symptoms using OMT, they may have a chance to avoid surgery.”
Osteopathic neuromusculoskeletal medicine is not as well understood by patients and other medical specialists as it could be, Dr. Rakowsky says.
“Osteopathic neuromusculoskeletal medicine specialists have expertise in biomechanical evaluation, and that includes observation, a movement exam, a structural exam, and an exam with the hands feeling for structures that are too tight, too loose, tender, swollen or not lined up properly,” she says. “Once we have an examination and we understand what the tissues are doing, we use hands-on manipulative techniques plus sometimes exercise prescription. We sometimes refer patients to physical therapy or occupational therapy to help the person bring their body structures back into their most balanced condition.”
Although people are less familiar with osteopathic manipulative medicine than with physical therapy, some of the same principles apply.
Advertisement
“People know their knee is supported by muscles, and they'll go to physical therapy to make their knee feel better. Well, the eye socket is bony but also muscular, and eyes are centered in the eye socket by a ring of muscles. That ring needs to be balanced, and OMT may help with that.”
Graves’ disease can cause thickening of fat and muscle structure behind the eyes, causing the eyeballs to be pushed forward and resulting in the sensation of tightness and pressure.
If a patient is not wearing contacts and doesn’t have glaucoma, Dr. Rakowsky can gently contact the eyeball through the lid, as well as the socket, to achieve more balance in those muscles.
“When I put my hand on the eye socket and eyeball and I evaluate for freedom of movement, bring them to balance, wait until the muscles that shut the eye and move the eye become even and feel symmetric,” she says. “That feels better to the patient.
Dr. Rakowsky’s patient with GO was a good candidate for treatment. The patient had not experienced adverse side effects from previous OMT for her neck and back pain.
“She was unlikely to experience a migraine headache or be sore or nauseated after treatment,” says Dr. Rakowsky. “Those side effects are rare in my practice, but I always consider whether the patient is likely to do well or to have trouble.”
In addition, Dr. Rakowsky has deep experience with cranial anatomy and osteopathic cranial manipulative medicine.
“I am familiar with treating problems in facial structures. This includes migraine headaches, trigeminal neuralgia, sinus pressure, jaw pain,” she says. “When people come in with eye pressure, I apply the same anatomic concepts to do the exam and figure out where their eye socket is tight. Then I use some of the same techniques and principles that work for common problems to help this less common problem.”
Advertisement
Dr. Rakowsky urges clinicians to consider OMT for patients with Graves’ eye disease, especially those who cannot tolerate or afford medication or surgery. She also notes that it is important that osteopathic neuromusculoskeletal medicine specialists collaborate with specialists who are treating the patient for other conditions.
“The physicians in the Osteopathic Neuromusculoskeletal Division want to work with those specialists,” she says. “They're essential. We want to augment the standard of care so that we can help the patient improve faster and live a better life.”
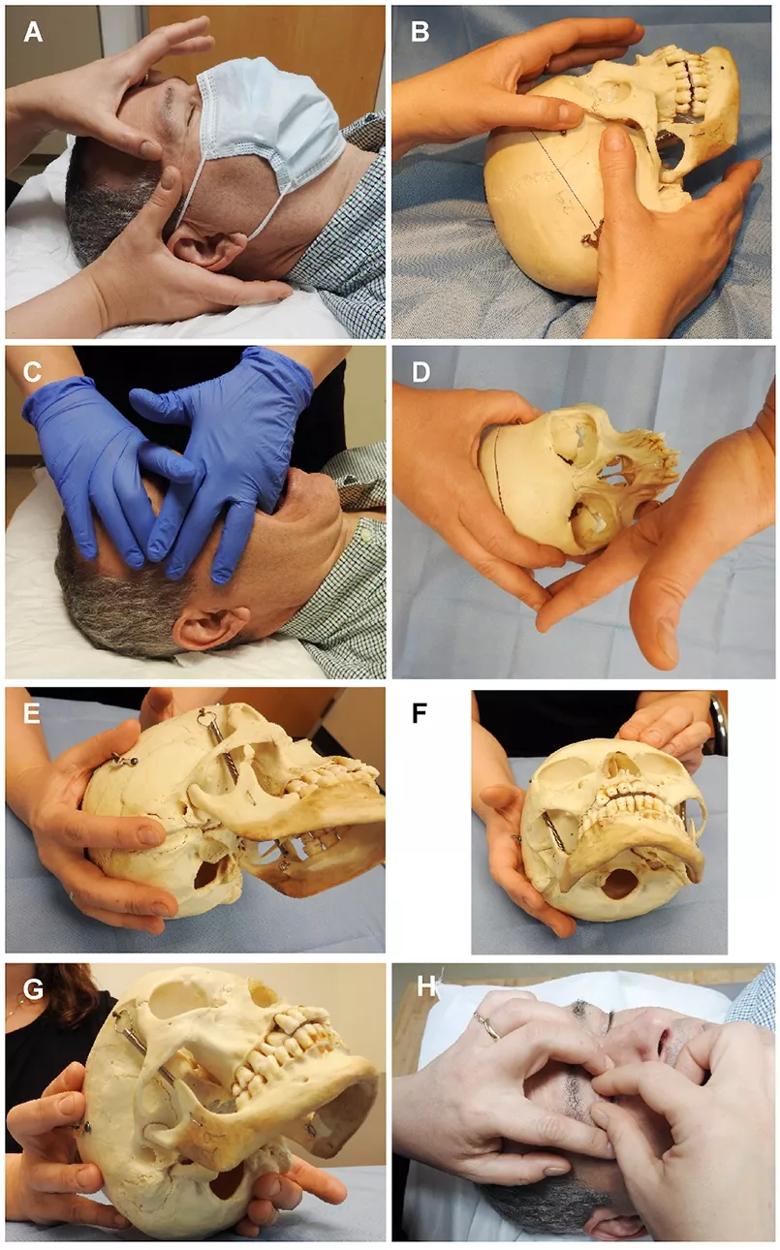
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0f70ef2f-4547-459e-8e5f-f81632ee75f2/Osteopathic-Treatment-Group)
OMT is used to increase fluid drainage and release restrictions in the orbit for patients with Graves’ ophthalmopathy. A-B) external cant hook; C-D) intraoral cant hook, E− F) V spread (occipitomastoid) suture, G) basion technique, H) indirect myofascial release of the orbit, including balancing tension on the globe. (These images were first published in the International Journal of Osteopathic Medicine.)
Advertisement
Advertisement
Compassion, communication and critical thinking are key
Registry data highlight visual gains in patients with legal blindness
Add AI to the list of tools expected to advance care for pain patients
Cleveland Clinic study investigated standard regimen
Despite the condition’s debilitating, electric shock-like pain, treatment options are better than ever
Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs
Program participation correlates with reduced use of opioids, X-rays and ED visits
The advanced stage of diabetic retinopathy is among the most challenging for retinal surgeons