Introduces at-home work and new patient screening tool

Reducing patient readmissions is a priority of case management teams at Cleveland Clinic. One year ago, case management leaders at Cleveland Clinic Hillcrest Hospital launched a pilot program to see how potential staffing, operations and process changes could help reduce readmissions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our case managers were already very cognizant of length-of-stay challenges, but we wanted to take a deeper look at why patients were getting readmitted, specific patient needs in the hospital, and what we could do differently in support of true care coordination,” says Cathy Pappin, MSN, RN, CCM, Manager of Case Management at Hillcrest Hospital.
Pappin believed that there were opportunities for improvement through working with other case management leaders in the healthcare system.
For example, at Hillcrest, case managers assessed all admitted patients. Depending on patient volume and length of stay, which was sometimes as short as one day, case managers weren’t always able to assess patients until they were nearing discharge or already discharged – on average, 20 hours after admission. Many patients didn’t need a full case-management assessment.
“When we thought about what we wanted from the pilot, one of the premises was to focus our assessments only on patients with post-acute needs,” Pappin says. “Roughly 55% of patients pre-pilot were going home without post-acute services like facility or acute rehab transfers, hospice or home care. We knew that time could be better spent caring for acute patients who needed our help most.”
Pappin also wanted the pilot to address improvements for identifying the most appropriate discipline – nursing or social work – based on the patient’s needs. “Too many times, the decision of what discipline would care for a patient was left in the hands of the team members working that day, and it wasn’t as objective as it should have been,” Pappin says.
Advertisement
Another key area of focus was post-discharge support and follow-up.
“A big contributor to patient readmissions is when patients have serious medical or mental health problems, but don’t have proper care established,” she says. “It’s important to connect these patients with community resources and ensure they follow their medical plan of care.”
After several months of planning, the case management pilot program was introduced on Hillcrest’s seven Medicine Institute units.
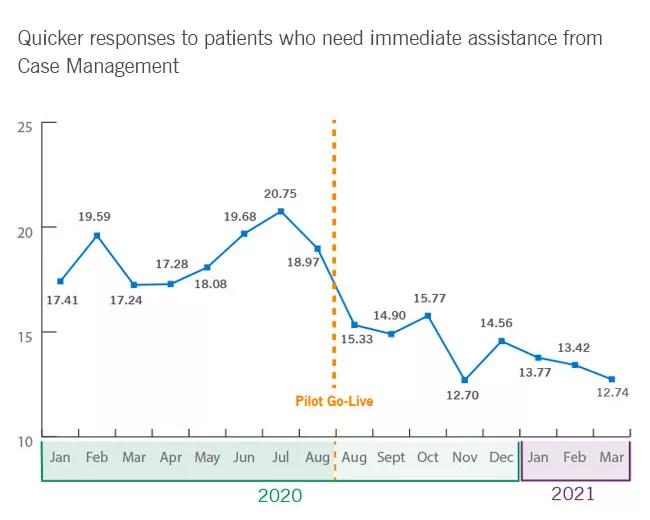
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2c9cbb86-2fde-49b5-8cbc-9f40da828512/CaseAssessmentGraph-inset_650x520_jpg)
Because of the COVID-19 pandemic, Hillcrest case managers were already working differently, which allowed Pappin to launch the pilot with a new staffing strategy. She created three new RN case manager work-at-home positions whose roles were to support and complement the inpatient case managers, Pappin says.
By screening for specific needs, the number of assessments dropped nearly 20 percent. This allows the team to focus their time on acute-needs patients. Pappin also says the team’s HCAPHS scores have exceeded initial benchmarking goals.
The next phases of the pilot will include increasing remote case management staff, expanding to all specialty nursing floors, incorporating the screening process in the emergency department, and eventually, developing and integrating a full case management care model redesign.
“My hope is that this becomes our way of life,” says Pappin.
Advertisement
Advertisement

Planning continues with critical, patient-focused input from nursing teams

Strengthening care through targeted resources and frontline voices

Embracing generational differences to create strong nursing teams

CRNA careers offer challenge and reward

An unexpected health scare provides a potent reminder of what patients need most from their caregivers

Cleveland Clinic Abu Dhabi initiative reduces ICU admissions and strengthens caregiver collaboration

Veteran nurse blends compassion, cutting-edge transplant training and military tradition to elevate patient care

Embrace coaching and other tips to be a stronger leader