SSRI exposure requires special staff, individualized care

Managing depression during pregnancy can create many challenges for both physicians and patients. Some experts recommend continuing medication in patients with severe depression and replacing or augmenting medication with psychotherapy. However, the use of antidepressant medications during pregnancy is controversial since it has not been adequately studied by medical researchers. Therefore, physicians may lack definitive answers to patient questions related to antidepressant use and pregnancy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
According to a 2008 study, about 5.6 percent of women in the U.S. use selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) during pregnancy. While there’s extensive literature related to the effects of in-utero exposure to SSRIs on term infants, there’s minimal data available related to the specific effects of SSRIs on preterm infants.
To help physicians improve pregnancy care that includes depression management, Cleveland Clinic recently completed a retrospective cohort study at Hillcrest Hospital, a tertiary care medical facility of Cleveland Clinic health system. For the first time, the study analyzed the oxygen levels and specific respiratory support needs of preterm infants affected by exposure to SSRIs during pregnancy. According to Principal Investigator Firas Saker, MD, FAAP, the results of the study will help physicians to “balance medication needs during pregnancy while individualizing both prenatal and neonatal patient care.”
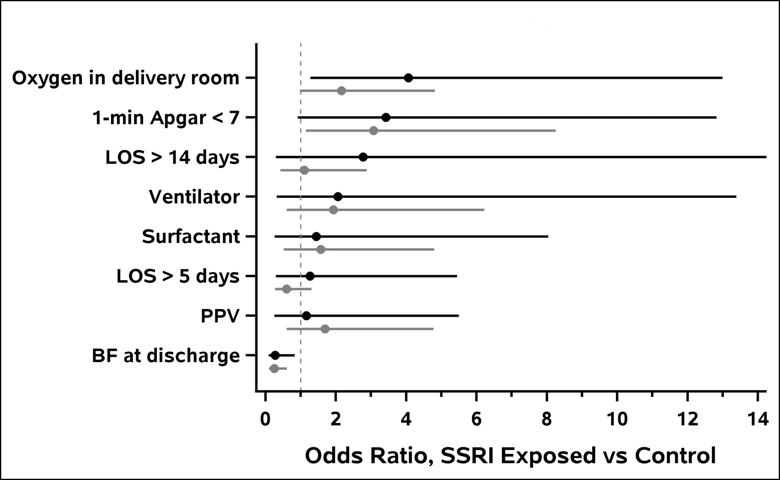
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d85a2101-039f-4595-bda2-178ee96234d1/Figure1_PretermNeonates_png)
Figure 1: Preterm neonatal odds ratio (unadjusted and adjusted odds ratio for outcomes).
To complete the study, Dr. Saker collaborated with Mary Temple-Cooper, MS, PharmD, BCPS, FCCP, as well as other experts from the Department of Pharmacy Services (Hillcrest). The team also included Sarah Worley from the Department of Quantitative Health Sciences and experts from the Department of Neonatology at Cleveland Clinic Children’s. The team reviewed electronic medical records from neonates born over a seven-year period, including neonates of mothers who were treated with SSRIs or venlafaxine, a type of SNRI, during pregnancy.
Advertisement
The primary endpoint of the trial was five-minute Apgar scores. Secondary endpoints included one-minute Apgar scores, oxygen and positive pressure ventilation use in the delivery room, oxygen requirements outside of the delivery room, breastfeeding at discharge and NICU admission.
A total of 168 neonates (51 preterm neonates and 117 term neonates) were exposed in-utero to SSRIs during the study period. These SSRI-exposed neonates were compared to a matched control group of term to preterm neonates. After adjusting for baseline characteristics and gestational age, Dr. Saker’s team reported the following key findings:

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/90d0a683-a1b2-412e-9424-ac24c5f9d8e3/18-CHP-225-SSRI-Visual-Abstract_jpg)
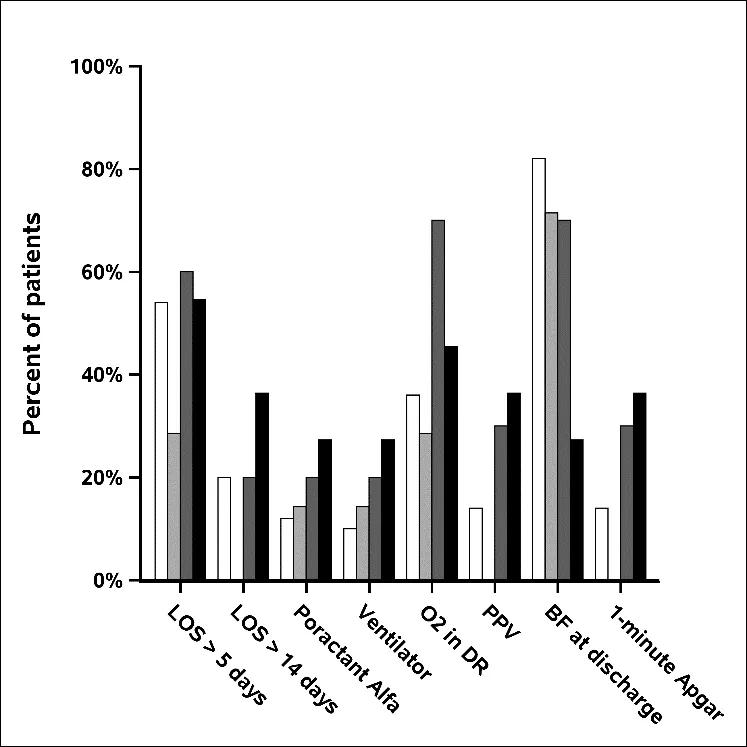
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/52fde371-6acd-4aee-94a9-6837d2940155/Figure2_EffectSertralineDosePretermNeonate_png)
Figure 2: Effect of sertraline dose on preterm neonatal outcomes (stratified by dose). White: control; light gray: 1–25 mg; dark gray: 50 mg; black: > 50 mg.
Cleveland Clinic currently allocates hospital staff members for various levels of delivery room needs. For example, specially trained staff are available to assist with neonatal resuscitation.
Advertisement
“Our findings of lower Apgar scores and an increased need for positive pressure ventilation at preterm birth underscores the need for experts in neonatal resuscitation during the delivery of SSRI-exposed neonates,” explains Dr. Saker. “Therefore, SSRI exposure should be considered an additional risk factor to account for when allocating delivery room staff. It’s especially important to plan for a higher level of appropriately trained staff when SSRI exposure is high.”
According to Dr. Saker, further studies are needed “to correlate the safety of lower than 100 mg sertraline [a type of SSRI] with poor neonatal outcomes.” In addition, he notes that “larger subgroup stratification by dose in a large prospective trial may help reveal the definitive dose responsible for poor neonatal outcomes.” By identifying alternative antidepressants medications and/or doses that are safer to use during pregnancy, physicians hope to individualize patient care and improve neonatal outcomes.
Advertisement
Advertisement

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity

Psychological care can be a crucial component of medical treatment