Application to flutter found safe and effective in study of 300+ patients
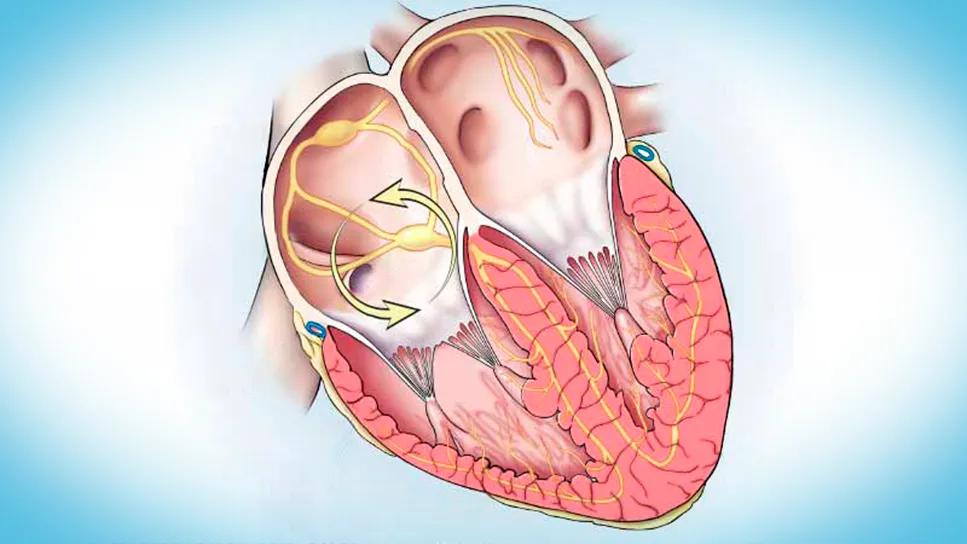
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bc853b03-a3e6-4cb7-bc06-eece8b1d698b/atrial-flutter-cqd)
heart illustration with circular arrows in right upper chamber
Pulsed field ablation (PFA) — an increasingly used nonthermal alternative to radiofrequency ablation (RFA) or cryoablation for treating atrial fibrillation (AF) — can be extended to address atrial flutter (AFL) as well, demonstrating acute success rates above 96% and favorable safety. So found Cleveland Clinic electrophysiologists in a prospective observational study of patients treated with PFA concomitantly for AF and atrial flutter.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study was recently published online ahead of print in JACC: Clinical Electrophysiology.
“In our experience, PFA catheters designed for treating atrial fibrillation have the versatility to successfully ablate sites for atrial flutter as well,” says the study’s senior and corresponding author, Ayman Hussein, MD, of Cleveland Clinic’s Section of Cardiac Electrophysiology and Pacing. “In this study, which is the largest single-center investigation of PFA for atrial flutter, we found that the method offers a viable ablation strategy while avoiding risks inherent in thermal techniques.”
“In our series, ablation of atrial flutter was acutely successful with a very low rate of recurrence,” adds co-investigator Oussama Wazni, MD, MBA, Section Head of Cardiac Electrophysiology and Pacing.
Thermal ablation, although effective for treating both AF and AFL, risks damage to neighboring structures. In addition, durability can be a problem, especially for anatomically complex targets. The use of PFA, with its nonthermal method of action, is rapidly expanding due to its safety and ability to cover large areas to increase likelihood of durability. PFA, being a faster ablation method, also has the advantage of requiring less anesthesia time.
PFA was initially approved for pulmonary vein isolation in AF and is now being explored for other uses, including cavotricuspid isthmus (CTI)-dependent and perimitral AFL.
The cohort — obtained from a prospectively maintained registry — included 311 patients (median age of 71 years; 71% male; 67% first-time ablation) at Cleveland Clinic between February and November 2024 who underwent PFA concomitantly for AFL and clinically indicated AF. Linear ablations for AFL were performed only in patients with documented flutters or in those who developed them during AF ablation.
Advertisement
The presenting rhythm was AF in 79 patients (25%), AFL in 103 patients (33%), sinus rhythm in 124 (40%) and paced rhythm in 5 (2%). Almost all patients (92%) were taking a direct oral anticoagulant; 7% were on warfarin. Patients were maintained on continuous oral anticoagulation therapy for at least three weeks before ablation and stayed on it thereafter without interruption.
A total of 368 AFL circuits were targeted. These included:
Every procedure employed constant use of intracardiac echocardiography to ensure optimal tissue contact with the PFA catheter; mapping of AFL was performed using electroanatomic mapping systems and high-density mapping catheters.
All PFA catheters used were FDA-approved for AF ablation.
Procedural success was defined as bidirectional block across ablation lines and termination of AFL. All targeted AFL circuits were successfully ablated, but adjunctive RFA was required in 3.5% (mostly perimitral circuits). The acute procedural success rate using PFA alone was 96.5% (99.5% for CTI-dependent flutters and 85.4% for perimitral circuits).
Other circuits that were successfully ablated using only PFA included those that were roof-dependent, around the pulmonary veins, scar-dependent, posterior wall-dependent, septal, anterior wall-dependent, around the superior vena cava, involving the Bachman’s bundle, left atrial appendage-related, near the coronary sinus and near the lateral tricuspid annulus.
Advertisement
Freedom from procedure-related adverse events was achieved in 99% of cases. There were no deaths, procedure-related cerebrovascular events, or cases of kidney failure, pericardial effusion requiring intervention, pericarditis or phrenic nerve injury. Major complications occurred in two patients, both involving vascular injuries requiring intervention. Four patients were readmitted within 30 days.
The patients who underwent PFA-only ablation (consisting of 355 circuits) were followed for a median of 175 days. AFL recurred in 14 circuits (3.9%), with a higher recurrence rate for perimitral flutters (10%) than for CTI-dependent flutters (1.5%).
Dr. Hussein emphasizes that PFA has worked well for AFL despite that fact that circuits — especially those that are perimitral — tend to be more complex than those for AF.
“Informally, colleagues outside of Cleveland Clinic have told me that when performing PFA for atrial fibrillation, they tend to switch to an RFA catheter if they encounter atrial flutter,” he notes. “In our experience, we can achieve good success by continuing ablation with the same PFA catheter to address flutter.”
For patients who need ablation solely for AFL, Cleveland Clinic electrophysiologists use thermal methods.
“Thermal ablation for atrial flutter is the gold standard except for high-risk patients, so we use it unless we are conducting PFA for atrial fibrillation in the same procedure,” Dr. Hussein explains. “It’s possible that down the road, the availability of new catheters designed more specifically for atrial flutter will open the door for PFA for this indication alone.”
Advertisement
He adds that the Cleveland Clinic team frequently evaluates new PFA catheter designs and PFA dosing regimens. He feels that smaller-footprint focal catheters have potential to be especially well suited to successfully ablate atrial flutter in patients with or without atrial fibrillation.
“This study sets the stage for future device innovation, long-term follow-up, procedural standardization and clinical trials,” Dr. Hussein says. “These are critical steps for widespread adoption of PFA for atrial flutter and its incorporation into guidelines.”
Advertisement
Advertisement
Study identifies a cohort of low-risk patients, finds LVEF predicts late VT/VF in those at higher risk
Nonthermal method promises faster procedure times, less risk to adjacent structures
Scenarios where experience-based management nuance can matter most
LAA closure may be compelling option in atrial fibrillation ablation patients at high risk of both stroke and bleeding
UK experts compare and contrast the latest recommendations
New analyses confirm preservation of ablation outcomes, broaden data on bleeding benefits
As use for atrial arrhythmias surges, studies turn to ventricular arrhythmias
While results were negative for metformin, lifestyle counseling showed surprising promise