As use for atrial arrhythmias surges, studies turn to ventricular arrhythmias
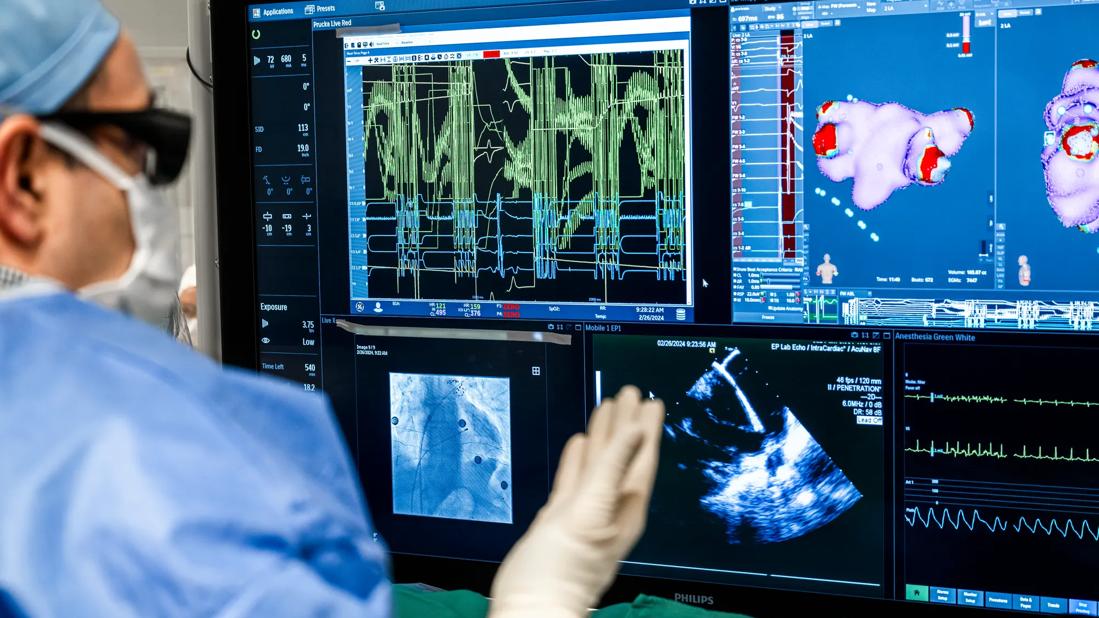
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/08c45478-a893-47ce-b0d5-cc0067f82a28/CCC_4654080_02-26-24_126_MLC-jpg)
physician watching monitor screens during an electrophysiology procedure
Increasing use of pulsed field ablation (PFA) has ushered in a safer age in arrhythmia management. Because of the nonthermal energy source’s selective nature, accidental damage to the esophagus, phrenic nerve or blood vessels — devastating and life-threatening risks seen with traditional radiofrequency ablation (RFA) and cryoablation methods — are unlikely to occur. An array of catheter-based PFA systems for atrial ablation are now commercially approved in the United States, and applications for ventricular arrhythmias are actively being explored.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Cleveland Clinic is a tertiary referral center in the U.S. for both atrial and ventricular ablation, and we perform more than 1,500 cases annually,” says Pasquale Santangeli, MD, PhD, Associate Section Head and Director of the Ventricular Tachycardia Program in the Section of Cardiac Electrophysiology and Pacing. “We now routinely use PFA for atrial ablation, and we are conducting research aimed at improving the technology and expanding its use to ventricular arrhythmias.”
This article provides an update of clinical applications in this rapidly changing field; for background on PFA technology, see this Consult QD summary from last year.
PFA is now used in many major U.S. medical centers to treat both paroxysmal and persistent atrial fibrillation. Enhanced safety is a key reason for its adoption in this setting, says Arwa Younis, MD, a clinical fellow in electrophysiology at Cleveland Clinic who will soon join the professional staff.
“Ablation of atrial fibrillation or flutter is an elective procedure,” Dr. Younis says, “so it is especially tragic if a patient ends up with a bad outcome, yet this can occur with even the most experienced radiofrequency ablation operators. Avoiding such an outcome in even one in 1,000 treated patients is worth the added expense to switch to PFA.”
Dr. Younis notes that learning to use this new technology is generally easy for RFA operators, as target precision is less important because of the reduced risk of damaging nontarget tissue.
He mentions that Cleveland Clinic electrophysiologists routinely use two PFA systems:
Advertisement
In Cleveland Clinic’s experience, there have been no occurrences of esophageal damage, stroke, nerve palsy or pulmonary vein stenosis with either of these two systems.
Dr. Younis notes that because PFA can be performed more rapidly than RFA, using less irrigation and requiring shorter procedures with less anesthesia time, it offers atrial ablation as a potential option to sicker patients.
More PFA systems with design improvements are rapidly entering the market, with manufacturers focused on making ablation even faster and more maneuverable. Cleveland Clinic is participating in multiple trials testing new catheter systems and evaluating expanded indications for current systems.
“The demand for atrial ablation is likely to increase in the coming years as the population ages, and I expect that most electrophysiologists who perform the procedure will soon be using PFA,” Dr. Younis predicts. “With PFA’s safety, speed and demonstrated noninferiority to thermal ablation techniques in terms of efficacy, it makes sense to switch over, in terms of both patient safety and economics.”
Although not yet approved by the FDA for commercial use, PFA for ventricular arrythmias is an active area of research at Cleveland Clinic. Dr. Santangeli’s group has conducted efficacy and safety comparisons of PFA and RFA in swine models, targeting common left ventricular arrhythmia locations (JACC: Clin Electrophysiol. 2024; 10[9]:1998-2009). They report that PFA had the advantages of producing deeper lesions with fewer steam pops (a complication caused by gas vaporization and an indicator of localized tissue destruction).
Advertisement
“We’re much earlier in the process of applying PFA to treat ventricular arrhythmias compared with atrial arrhythmias,” Dr. Santangeli says. “But we are excited about its potential uses, especially because of PFA’s tissue selectivity and its potential ability to go deeper in tissue than RFA can, producing more complete ablation.”
Dr. Santangeli adds that PFA’s advantages — including not requiring a high volume of saline irrigation to control heat and the reduced time needed to perform ablation compared with thermal methods — are especially critical for people with ventricular arrhythmias, many of whom have heart failure and are less likely to tolerate more complicated prolonged procedures.
Cleveland Clinic electrophysiologists are making inroads into clinical applications in humans, under FDA exemptions for compassionate use. They have used PFA for ventricular tachycardia (VT) refractory to other treatment and for severe symptomatic isolated premature ventricular contractions. Such arrhythmias frequently have a deep origin in the intraventricular septum, from the left ventricular summit or papillary muscles, which PFA is likelier than thermal methods to reach and ablate.
Of note, Cleveland Clinic recently published two case reports of the first use of PFA to successfully address ventricular arrhythmias associated with complex substrates:
Advertisement
Dr. Santangeli is principal investigator of the ASCEND pilot study (NCT06891456), which is evaluating the safety and efficacy of PFA (using Boston Scientific’s FARAPOINT™ catheter) compared with standard RFA for drug-refractory VT. This randomized, controlled, open-label study is currently enrolling 40 patients at Cleveland Clinic who have ischemic cardiomyopathy after myocardial infarction and an implantable cardioverter-defibrillator. The trial is expected to be completed by the end of 2028.
Meanwhile, enrollment has begun in a multicenter study of Medtronic’s PFA system and catheter that will combine radiofrequency and pulsed field waveforms for the treatment of sustained VT in patients with ischemic cardiomyopathy. Cleveland Clinic is a participating center.
“PFA is a powerful tool that has been demonstrated to be safe and effective for atrial ablation and has great potential to treat ventricular arrhythmias,” Dr. Santangeli concludes. “But we also must proceed with caution to define targets and detect possible complications through research.”
Dr. Santangeli is a consultant to, and has received research grants from, Medtronic, Biosense Webster, Abbott and Boston Scientific. Dr. Younis has received research grants from Boston Scientific.
Advertisement
Advertisement
Scenarios where experience-based management nuance can matter most
Application to flutter found safe and effective in study of 300+ patients
Large, multinational trial finds no significant difference in vigorous versus nonvigorous exercise
Study identifies a cohort of low-risk patients, finds LVEF predicts late VT/VF in those at higher risk
JAMA study adds new data to decades-long guidance
Nonthermal method promises faster procedure times, less risk to adjacent structures
$14M NIH grant supports research toward medications to prevent progression
Document addresses screening and treatment while underscoring need for more randomized data