Study identifies a cohort of low-risk patients, finds LVEF predicts late VT/VF in those at higher risk
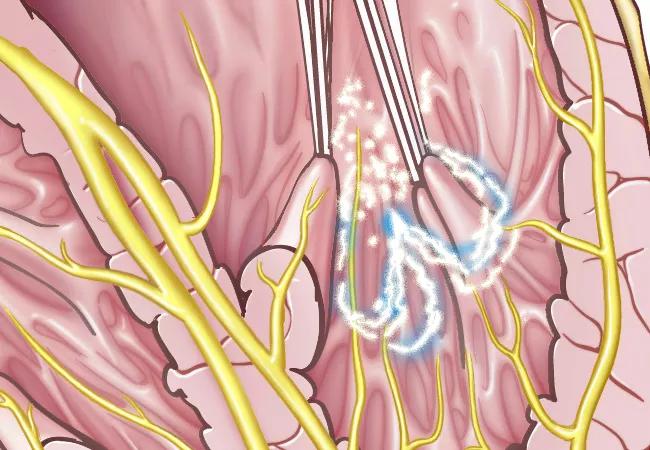
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0528ba1a-1709-4be7-af58-d391c65227d9/18-HRT-070-Wazni-CQD_jpg)
ventricular tachycardia
Late ventricular tachycardia (VT) and ventricular fibrillation (VF) are relatively common in the immediate post-treatment period among patients with acute ST-segment elevation myocardial infarction (STEMI). However, few such events result in cardiac arrest in individuals who have received timely primary percutaneous coronary intervention (PCI).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So finds a new national cohort study published in JAMA Network Open (2024;7[5]:e2410288), which examined outcomes in a large population treated with contemporary reperfusion protocols.
“Our results show that, in patients with STEMI undergoing primary PCI, late VT or VF associated with cardiac arrest is rare, particularly if patients are lower-risk,” says senior author Jacqueline Tamis-Holland, MD, Director for Acute Coronary Care in Cleveland Clinic’s Section of Invasive and Interventional Cardiology. “Decreasing LVEF is the most significant factor associated with late ventricular arrhythmias with cardiac arrest in this overall population of patients.”
VT or VF occurring more than 24 hours post-reperfusion is rare but can be life-threatening in patients with STEMI, according to literature reports. Little research exists about the incidence and timing of such events in an era of contemporary PCI.
Current practice typically is at least two days of in-hospital telemetry for heart rhythm monitoring, regardless of a patient’s risk profile after STEMI. However, guidelines are lacking about the optimal length of monitoring and timing of discharge.
Dr. Tamis-Holland and colleagues aimed to fill that evidence gap using data from patients with STEMI treated with PCI from January 2015 through December 2018 in the National Cardiovascular Data Registry (NCDR) Chest Pain–MI Registry. Among the cohort, they assessed the incidence and timing of VT or VF events and in-hospital mortality associated with late VT or VF, along with identifying factors associated with these complications.
Advertisement
A total of 174,126 adults with uncomplicated STEMI treated at 814 U.S. sites were identified from the registry. Late VT was defined as a run of seven or more beats of VT during STEMI hospitalization at least one day after PCI, and VF was defined as any episode of VF at least one day after PCI.
“To our knowledge, this study represents the largest such population examined to date and encompasses a contemporary cohort with STEMI treated promptly with primary PCI,” Dr. Tamis-Holland notes.
Outcomes were assessed both in the overall cohort and in a predefined subpopulation of patients with uncomplicated STEMI (n = 99,905; 57.4%), defined as those without prior MI or heart failure, systolic blood pressure below 90 mmHg, cardiogenic shock, cardiac arrest, reinfarction or left ventricular ejection fraction (LVEF) below 40%.
Any VT or VF was reported after primary PCI in 15,460 patients (8.9%) in the overall cohort and in 5,432 patients (5.4%) in the subgroup with uncomplicated STEMI. Late VT or VF occurred in 2.4% of the overall cohort and 1.7% of the uncomplicated STEMI subpopulation.
Instances of late VT or VF associated with cardiac arrest were uncommon, reported in 0.4% of the overall cohort and 0.1% of patients with uncomplicated STEMI. At the same time, the risk of in-hospital mortality was significantly elevated in patients with late VT or VF relative to those without it, with adjusted odds ratios of 6.40 (95% CI, 5.63-7.29) in the overall cohort and 8.74 (95% CI, 6.53-11.70) in patients with uncomplicated STEMI.
Advertisement
In the overall cohort, numerous factors were significantly associated with development of late VT or VF, with reduced LVEF having the strongest association, followed by male sex, systolic blood pressure at admission and cardiogenic shock at admission.
In the overall cohort, reduced LVEF was also the most significant predictor of late VT or VF with cardiac arrest: the adjusted odds ratio for cardiac arrest with late VT/VF was 1.67 (95% CI, 1.54-1.85) for every 5-unit LVEF decrease below 40%. Other significant predictors of late VT/VF with cardiac arrest were difficulty crossing the lesion during PCI, heart failure at admission, cardiogenic shock at admission and three-vessel coronary artery disease.
“Our findings showed that identifying factors associated with any late VT or VF and cardiac arrest is challenging,” says Dr. Tamis-Holland, “but identifying factors associated with any late VT or VF with cardiac arrest can be achieved with greater accuracy and specificity.”
Despite advances in primary PCI and systems of care for patients with STEMI, the researchers found a risk of VT or VF overall that was consistent with previous reports in patients with MI. However, late VT/VF associated with cardiac arrest was rare, particularly among the low-risk cohort of patients.
“These findings should be helpful in determining the duration of telemetry and length of stay in our patients with acute MI,” Dr. Tamis-Holland concludes. “Our hope is that they can help clinicians distinguish higher-risk patients who may benefit from longer inpatient monitoring from lower-risk patients who can safely undergo earlier discharge after successful reperfusion.”
Advertisement
“This study helps establish the rates of late VT/VF among STEMI patients undergoing primary PCI in a contemporary registry,” adds Venu Menon, MD, Cardiac Intensive Care Unit Director at Cleveland Clinic, who wasn’t involved in the study. “Awareness of the incidence and factors associated with these life-threatening arrhythmic events is important, as many STEMI patients are no longer admitted to the cardiac ICU and length of stay continues to decrease in this clinical setting.”
Advertisement
Advertisement
Application to flutter found safe and effective in study of 300+ patients
Nonthermal method promises faster procedure times, less risk to adjacent structures
Scenarios where experience-based management nuance can matter most
Consortium makes key recommendations to improve prevention practices
As use for atrial arrhythmias surges, studies turn to ventricular arrhythmias
Large, multinational trial finds no significant difference in vigorous versus nonvigorous exercise
In the wake of NOTION-3 findings, a strong argument for physician judgment remains
Transvalvular LVAD support transforms emergency surgery into urgent procedure