ILAE advises emphasizing options for patients with drug-resistant epilepsy
Most patients up to age 70 with drug-resistant epilepsy should be offered surgical evaluation, and even those who are seizure-free on antiseizure medications with a resectable lesion might benefit from surgery by avoiding drug side effects. That’s the advice of the International League Against Epilepsy (ILAE) in a new consensus document published as a Special Report in Epilepsia designed to provide recommendations on the timing of referral for epilepsy surgery evaluation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Surgery for epilepsy offers patients the best chance of a cure, and delaying it in order to search for palliative options can lead to unnecessary consequences, including cognitive harm, poor psychosocial outcomes, and increased risk of morbidity and death,” says the document’s first and corresponding author, Lara Jehi, MD, an epilepsy specialist in Cleveland Clinic’s Epilepsy Center. Dr. Jehi led the work as Chair of the Surgical Therapies Commission for the ILAE, the highest authority in epilepsy care and research. “With these recommendations, we are hoping that more patients who could benefit will be more promptly offered this important option.”
The recommendations from the ILAE are the result of a Delphi consensus process involving 61 epileptologists, epilepsy neurosurgeons, neurologists, neuropsychiatrists and neuropsychologists from 28 countries with a median of 22 years in practice. The process involves a series of questions provided to the group, in which responses form the basis of the next round. Consensus was defined as 66% agreement, and three rounds were conducted to optimize agreement.
Such recommendations differ from clinical practice guidelines, which are based on rigorous systematic review of evidence. In contrast, consensus recommendations are used to provide guidance on controversial issues for which evidence is limited. “We met at least a dozen times over the course of 18 months to craft these recommendations,” notes Dr. Jehi. “Surgery is highly underutilized to treat epilepsy, and our team took care to consider all the possible scenarios that practicing neurologists struggle with as they determine whether or not to refer a patient for evaluation.”
Advertisement
Dr. Jehi identifies the following as some of the document’s key recommendations.
Advertisement
Consensus was not reached for referring patients for surgical evaluation in some clinical scenarios. These included:
The authors note that such controversies point to potential areas for research.
The ILAE statement emphasizes that many patients and even clinicians commonly have misconceptions about epilepsy surgery, leading to underutilization or unnecessary delay of surgery. They note that risks of surgery are often overestimated and negative impacts of poorly controlled seizures are often underestimated.
Dr. Jehi adds that surgical evaluation may lead to consideration of previously unexplored options, such as laser interstitial thermal therapy or neuromodulation for patients who are unsuitable for surgery. Referral for surgery evaluation for patients with drug-resistant epilepsy, she notes, has been demonstrated to be cost-effective, whether or not the patient actually undergoes surgery.
“Patients should be counseled that referral for surgical evaluation is not in any way a commitment to undergo brain surgery,” says Dr. Jehi. “For those who are not surgical candidates, evaluation can lead to other benefits, such as improved diagnosis, better understanding of their condition and additional management strategies.”
Advertisement
Advertisement

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Patients with epilepsy should be screened for sleep issues

Sustained remission of seizures and neurocognitive dysfunction subsequently maintained with cannabidiol monotherapy

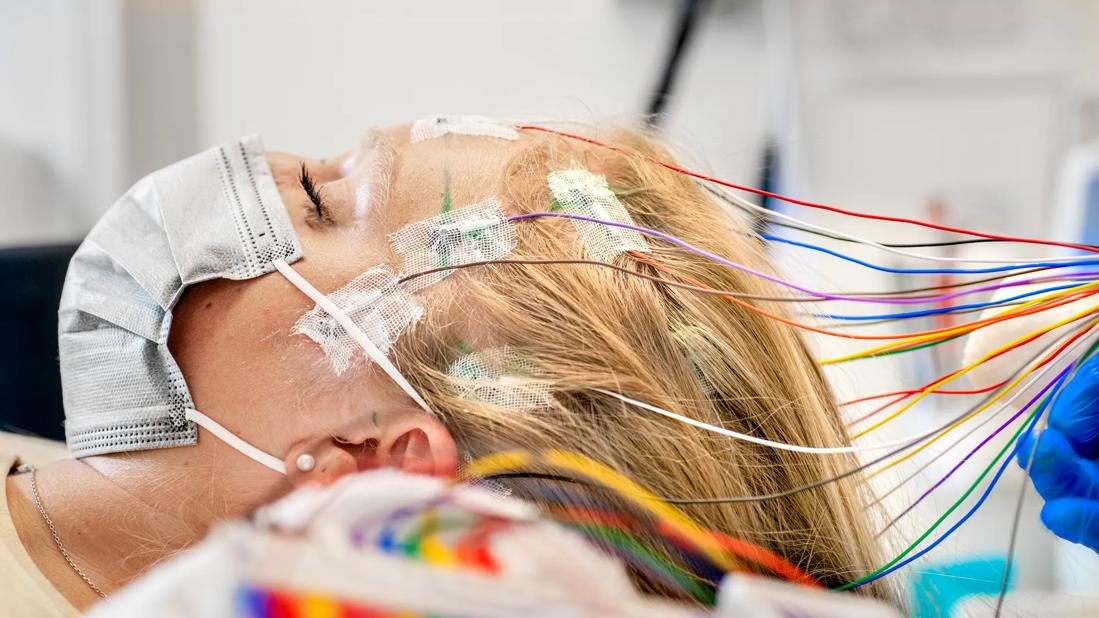
Model relies on analysis of peri-ictal scalp EEG data, promising wide applicability

Investigational gene approaches offer hope for a therapeutically challenging condition
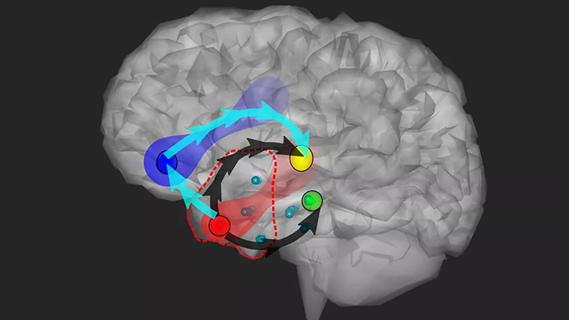
Study combines intracranial electrophysiology and SPECT to elucidate the role of hypoperfusion

Characterizing genetic architecture of clinical subtypes may accelerate targeted therapy

Data-driven methods may improve seizure localization and refine surgical decision-making