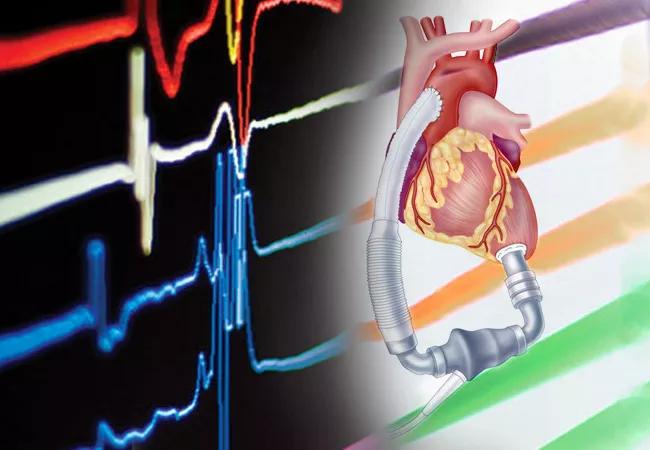
Three significant developments in the last five years have changed the way the heart failure specialists at Cleveland Clinic in Florida evaluate and select patients as potential candidates for left ventricular assist device (LVAD) therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
According to Jerry D. Estep, M.D., FACC, FASE, Chairman of Cardiology at Cleveland Clinic Florida and a leading heart failure researcher, the latest device outcomes data, a new risk assessment process, and the development of decision support tools have refined the team’s approach.
“Some patients with end-stage heart failure do exceptionally well with LVAD therapy, enjoying a survival advantage and quality of life improvements,” says Dr. Estep, who has played key roles in major studies of mechanical circulatory support devices throughout his career. “Selecting the right patients, however, is key to achieving these desired outcomes.”
Over 6 million adults in the United States have heart failure, reports the Heart Failure Society of America. It is the number one cause of hospitalizations in the Medicare population and accounts for approximately 1 million hospitalizations annually.
Treatment options for end-stage heart failure include heart transplant and LVAD therapy. While heart transplantations have increased consistently in recent years, climbing to 4,169 transplants in 2022, only 2,464 primary LVADs were implanted in 2021, according to the latest annual report from The Society of Thoracic Surgeons (STS) Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS). Although this is down from the peak volume in 2019, there remains a great opportunity to use LVADs in select patients.
“Circulatory support devices were developed as a bridge to transplant but their purpose has evolved,” says Dr. Estep. “INTERMACS data show that 81% of patients are now implanted as destination therapy. This is important because many patients with advanced heart failure are not considered transplant candidates.”
Advertisement
Older patients (>70yo) with comorbidities, individuals with severe obesity independent of age, and those with pulmonary hypertension related to left-sided heart failure are just some of the patients that may benefit from LVAD, according to Dr. Estep. He is concerned, however, that many LVAD candidates are missing out on this durable option for life-extending care.
Contemporary outcomes support the durability of LVAD therapy. The STS-INTERMACS annual report indicates 1-year post-LVAD survival has reached 83% while 5-year survival has climbed to nearly 52%. Similarly, last year’s follow-up study of the pivotal MOMENTUM 3 trial, which compared the centrifugal-flow HeartMate 3™ (HM3) LVAD with the axial-flow HeartMate II in patients with advanced heart failure, calculated a 5-year survival of 58.4% in the centrifugal-flow group versus a 43.7% in the axial-flow group.
“HeartMate 3 is the most forgiving pump and the most hemocompatible,” asserts Dr. Estep, a senior leader in the MOMENTUM 3 trial and co-chair of its flow optimization subcommittee. “It has propelled us forward by eliminating pump-related thrombosis and significantly lowering stroke risk.”
He notes, “We now have LVAD 2-year survival rates comparable to those with heart transplantation.”
While generalized survival data with LVAD therapy is highly encouraging, having an individualized probability of survival can help patients and their families better understand the benefits and risks of LVAD implantation. Dr. Estep, as the senior author, was part of a team of researchers who used clinical data from the MOMENTUM 3 trial and a 2-year follow-up study (Continued Access Protocol) to develop and validate a personalized risk tool to accurately predict 1- and 2-year survival after implantation with the HM3 LVAD.
Advertisement
“Using six pre-implant clinical parameters, we are able to calculate a patient’s unique HM3 Survival Risk Score,” explains Dr. Estep. Outlined in the study published last December in the journal JACC: Heart Failure, those parameters include “demographic variables (age and prior sternotomy), laboratory data (serum sodium and BUN), an echocardiographic parameter (LVEDD reflective of LV size), and a hemodynamic finding (RAP/PCWP ratio).”
Dr. Estep highlights that low risk patients, as defined by this HM3 risk score, had a 2-year survival of approximately 91% after LVAD therapy, which he says is astonishing. “We now use this prediction tool to help guide patient selection and support shared decision making when we talk with patients and their loved ones about LVAD therapy,” he adds.
Likewise, the Cleveland Clinic Florida heart failure team offers LVAD candidates a number of decision support tools. As a senior author of the VAD Decision Aid (VADDA) trial, Dr. Estep helped create the LVAD Decision Aid, which is designed to increase patient knowledge on the risks, benefits, misconceptions and projected experiences associated with LVADs. “This tool helps our patients make informed decisions on accepting or declining LVAD placement,” says Dr. Estep. “It promotes important conversations and shared decision making, which is central to our ability to provide patient-centered care.”
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.