Risk aversion may be a factor in reduced transplant volumes

By Jesse D. Schold, PhD, MStat, MEd
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The benefits of kidney transplantation have been well documented for more than a decade. For the typical kidney transplant candidate, transplantation is associated with improved life expectancy, quality of life and reduced costs compared to maintenance dialysis.
Moreover, this benefit is applicable for patients with multiple comorbid conditions, in countries with diverse healthcare delivery systems, and with the use of donor organs with increased risk factors.
The primary barrier to kidney transplantation is the limited donor supply relative to the number of candidates.
From 1989 to 2006, the number of national solitary kidney transplants in the United States increased in each consecutive year (Figure 1). In 2006, there were 17,095 transplants performed, including 9,913 from deceased and 6,572 from living donors.
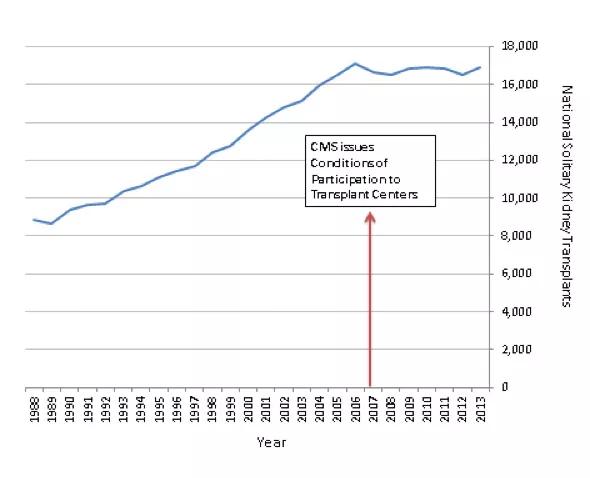
Figure 1. National Kidney Transplant Volume by Year
Since that time, the national volume of transplants has remained stagnant despite an increase in the number of candidates from 32,356 in 2006 to 36,396 in 2013. Currently there are more than 108,000 patients on the national kidney transplant waiting list.
A significant change in the field of kidney transplantation has been the increased impact of quality oversight. In 2007, the Centers for Medicare and Medicaid Services issued a Conditions of Participation for transplant centers that explicitly links transplant center performance, as measured by risk-adjusted graft and patient survival, with the availability of public funding. Centers that fail to meet these quality standards may lose Medicare support and are unlikely to continue to sustain a transplant program.
An important ongoing question is whether the stagnation in national transplant rates is associated with the increased emphasis on quality oversight. Members of the transplant community have raised this concern and one national study1 has demonstrated that, on average, centers that receive low performance evaluations significantly reduced their transplant volumes while other centers continued to increase rates during the same time period.
A potential mechanism for this relationship is that centers become risk- averse – less likely to accept candidates or donor organs with perceived heightened risk for poor outcomes. Importantly, because quality metrics are based on risk-adjusted models (accounting for many factors associated with graft loss and patient death), this type of risk aversion may or may not improve center performance but reduces access to care for candidates who may benefit from the procedure.
Quality assurance clearly has an important role in healthcare. The many emerging quality metrics are not unique to transplantation. Moreover, quality oversight likely provides important benefits to the field of transplantation.
However, there is probably a balance that should be struck between regulatory oversight and the potential (and unintended) reactions it may generate among healthcare providers.
In kidney transplantation, the wealth of empirical evidence suggests that increasing transplant rates has clear benefits for end-stage renal disease patients. The degree to which outcome quality regulation has impacted transplant rates is not completely clear but is important to monitor.
In addition, metrics that incentivize the growth of transplantation may be important to consider in conjunction with current outcome measures. In the end, prioritizing policies that stimulate access to transplantation – such as incentives for early referral and evaluation of candidates – likely will have the greatest public health benefits.
Dr. Schold is an associate staff member of Cleveland Clinic’s Department of Quantitative Health Sciences and Director of Outcomes Research for the Kidney Transplant Program. He can be reached at scholdj@ccf.org or 216.444.6254.

Smaller incision may lead to reduced postoperative pain for some patients

Improving access to lifesaving kidney transplant

The process could improve access and equity for patients with end-stage kidney disease
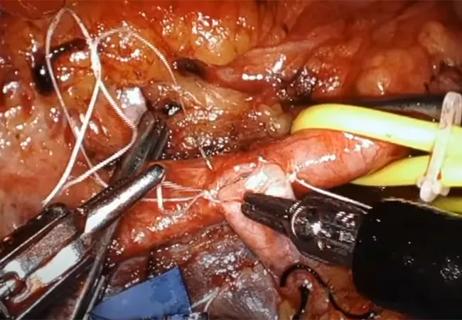
Video offers glimpse into technically challenging portion of the procedure

Infectious disease and kidney transplant specialists share key insights

Demographic and social factors found to influence preemptive listing

New interventions and policies haven’t increased wait-listing

Cleveland Clinic surgeons use single-incision robotic surgery to perform kidney transplant