The multi-institutional study found that adherence to four key metrics improves patient survival
New research indicates four process-related quality metrics are significantly associated with disease outcomes and mortality in oral cavity squamous cell carcinoma (OCSCC) patients. The findings from a multi-institutional cohort validate that adherence to all, or all but one, of the quality metrics is associated with improved survival. The study was published in the journal Head & Neck.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Over the past several years, there has been a movement towards the development of quality of care measures for patients with OCSCC. Previously published data from a single institution for oral cavity cancer assessed a variety of process-related metrics, and identified four quality metrics where compliance was associated with improved patient survival. These metrics, known as a “clinical care signature” include neck dissection with lymph node yield of 18 or more, no unplanned surgery within 14 days, no unplanned readmission within 30 days and referral for adjuvant radiotherapy for stage III or IV disease. The objective for the present study was to evaluate, in a multi-institutional cohort, if adherence to these four key metrics were associated with improved survival in patients with clinically treated OCSCC.
A multi-institutional retrospective review was performed of patients 18 years and older who were treated with primary surgical resection for OCSCC at three tertiary care centers between January 1, 2005 and January 31, 2015. The primary outcome assessed was the rate of adherence to the four quality metrics, and secondary outcomes assessed were measures of survival (overall [OS], disease-specific [DSS] and disease-free [DFS]).
“While these are all process-related metrics, I think that two of them really speak to the quality of immediate care,” says Eric Lamarre, MD, an otolaryngologist with Cleveland Clinic’s Head & Neck Institute and the lead author of the study. “The lymph node yield of 18 or more has been shown to speak to the extent of neck dissection performed. Referral to adjuvant treatment for stage III or stage IV is a very well accepted guideline – it speaks to the quality of the multidisciplinary care in the management of these patients.”
Advertisement
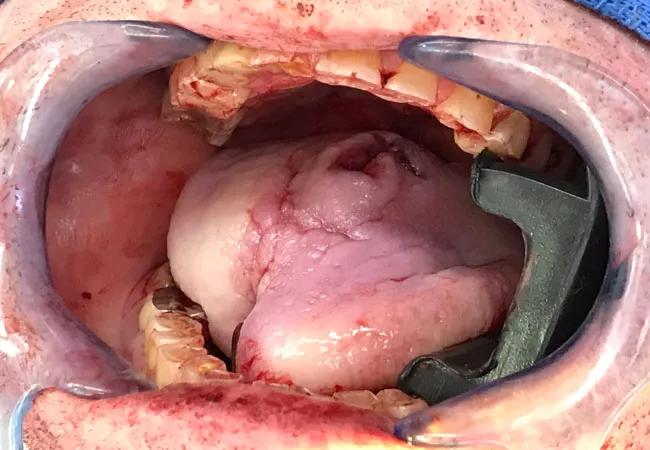
The study included 773 patients from 3 institutions. The patient cohort was comprised of 474 males (61.32%) and 539 patients (69.72%) were tobacco users. Oral tongue was the most common. Methods of surgical resection included wide local excision (20.83%), partial glossectomy (38.03%), total glossectomy (0.65%) or other composite resection (40.36%).
“One of the things that surprised me was the compliance,” says Dr. Lamarre. “Overall, I felt that compliance was quite strong. Even with strong compliance, we were able to determine that failure to comply with the metrics was significant enough to make our conclusions.”
Compliance with the quality metrics showed 507 patients (65.6%) met all four quality metrics of interest. There were 240 patients (31.1%) who had adherence to three of the four quality metrics, and 26 patients (3.4%) had two or more missing metrics. However, compliance with the individual quality metrics included overall was high. Seven hundred thirty-six patients (95.21%) did not have an unplanned reoperation within 14 days and 731 patients (94.57%) did not require readmission within 30 days. Five hundred ninety-five patients (76.97%) from the total cohort had a neck dissection with lymph node yield of 18 or greater, and of the 494 patients with stage III or IV disease 455 (92.1%) received a referral for radiation therapy.
“Interestingly, neck dissection with lymph node yield of 18 or greater was, by itself, not significantly associated,” says Dr. Lamarre. “There’ve been some studies to suggest that it may, so that was a bit of a surprising finding. Unplanned readmission was significantly associated with worse overall survival. Reasons for unplanned readmission may be the result of pre-existing comorbidities, surgical site complications, or difficulties with transitions of care. The only metric that demonstrated the improved disease-specific survival was referral to radiation oncology for late-stage oral cavity cancer.”
Advertisement
Looking ahead, Dr. Lamarre notes that the next steps for this research might be to find other similar disease processes within the head and neck to see if there are any process related-metrics that impact survival. He also believes that otolaryngologists need to examine how to improve adherence and compliance to these metrics through quality improvement programs.
“I think what this study does, is it validates these metrics in a multi-institutional cohort,” says Dr. Lamarre. “These four metrics are integral to the care of the oral cavity cancer patient and really speak to the quality of care of the disease process and also significantly impacts overall survival.”
Advertisement
Advertisement

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life

Study shows no negative impact for individuals with better contralateral ear performance

HNS device offers new solution for those struggling with CPAP

Patient with cerebral palsy undergoes life-saving tumor resection

Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition

Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.