Finding has potential to improve treatment
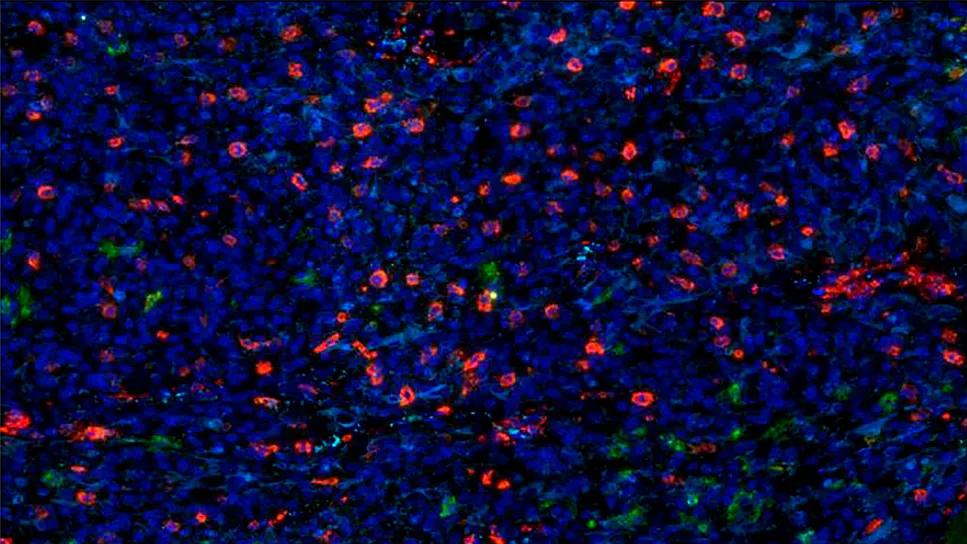
Breakthrough research conducted at Cleveland Clinic’s Lerner Research Institute sheds light on how certain cancer stem cells (CSCs) evade the immune system. As explained in a paper published on line January 12 in Cell Stem Cell, glioblastoma stem cells express a lower level of the innate toll-like immune receptor 4 (TLR4) than surrounding cells. Since TLR4 overexpression inhibits the proliferation of CSCs, low levels of TLR4 allow CSCs to persist and multiply, repopulating a tumor in a hostile microenvironment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“It’s like CSCs have their headphones on and have lost ability to sense the environment around them,” remarks Justin Lathia, PhD, the stem cell biologist whose lab was responsible for this finding.
The body is well equipped to target and eliminate cancer cells. Tumors emit hostile inflammatory signals that label them as damaged cells. These signals are picked up by toll-like receptors (TLRs), which rally the troops to mount an immune response.
Under normal circumstances, the immune system kills damaged cells and eliminates them. But for reasons not understood until now, glioblastoma cells do not elicit the same killing response. Their ability to evade the immune system and proliferate has made this form of brain cancer one of the deadliest.
While working on his doctorate in stem cell biology in the NIH-Cambridge Graduate Partnership Program, Dr. Lathia became involved in the role of TLRs in brain stem cells. When he started his own lab at Cleveland Clinic, he continued his investigation. “Since they played a key role in normal cell biology, I wondered if they could be important for brain cancer stem cells,” he says.
This question led Dr. Lathia, Dr. Alvaro Alvarado (a recent graduate of the Cleveland Clinic Molecular Medicine PhD program) and colleagues to discover that CSCs in glioblastoma have lost the TLR that allows them to sense damage and die or recruit immune cells. “This is an evolutionary advantage that allows them to grow and persist, despite their being damaged,” he says.
Advertisement
The exciting implication of this finding is that it opens the door for therapeutic options to treat glioblastoma.
Because achieving the overexpression of TLR4 would be difficult, it is unlikely to be a therapeutic target. However, the researchers also discovered that retinoblastoma-binding protein 5 (RBBP5) plays a critical role in the glioblastoma self-renewal process, and that eliminating this protein caused the tumor to collapse. Their finding adds to a 2016 finding that a different member of the RBBP family contributes to chemosensitivity in glioblastoma.
“This suggests that targeting this family may sensitize CSCs to damage signals, providing a unique therapeutic opportunity,” says Dr. Lathia.
This groundbreaking project was funded entirely through philanthropic support from Sontag Foundation, Blast Glioblastoma and Cleveland Clinic’s VeloSano Bike to Cure program.
Photo Credit: ©Greg Mueller
Advertisement
Advertisement

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists