Phase 3 study may lead to first FDA approval for the indication
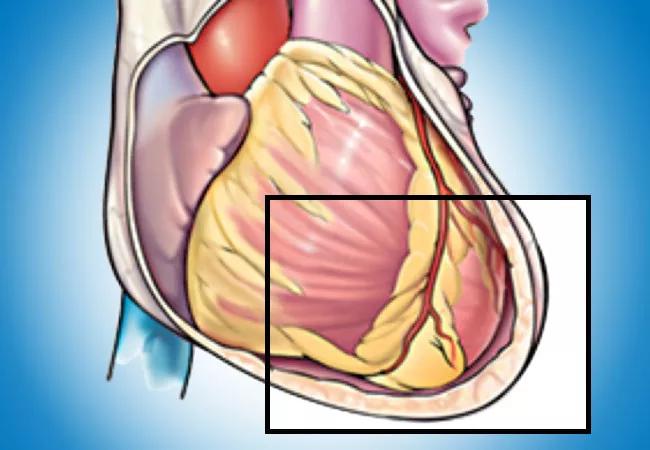
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ffc3497c-3d31-4ef9-aca0-92e2a1561c23/20-HVI-2006252-pericarditis-650x450-1_jpg)
20-HVI-2006252-pericarditis-650×450
Targeting interleukin-1 (IL-1) may represent a paradigm shift in the treatment of patients with recurrent pericarditis, suggest results from the phase 3 RHAPSODY trial presented at the virtual 2020 Scientific Sessions of the American Heart Association (AHA) and published simultaneously in the New England Journal of Medicine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The multicenter study evaluated rilonacept, an IL-1α and IL-1β cytokine trap, in patients with recurrent pericarditis. It found that the agent was associated with rapid resolution of active recurrent pericarditis episodes and a significantly reduced risk of pericarditis recurrence compared with placebo.
“Interleukin-1 has been implicated as an important mediator of recurrent pericarditis, a highly disabling disease with a huge clinical and economic burden and no current FDA-approved therapies,” says lead study author Allan Klein, MD, Director of Cleveland Clinic’s Center for the Diagnosis and Treatment of Pericardial Diseases. “Rilonacept represents a new targeted approach to recurrent pericarditis. Results of this pivotal study indicate this type of interleukin-1 blocker may be a game changer in the management of patients with this disease.”
The phase 3 RHAPSODY trial built on the findings of a successful phase 2 study of rilonacept for recurrent pericarditis presented by Dr. Klein at the AHA’s 2019 Scientific Sessions (recapped here).
RHAPSODY was designed as a double-blind, placebo-controlled, randomized withdrawal trial to determine time to first recurrence in the withdrawal period. The study enrolled patients with symptomatic recurrent pericarditis and systemic inflammation from Australia, Israel, Italy and the United States, with Cleveland Clinic’s academic research organization, C5Research, serving as the study’s coordinating center.
Patients aged 12 years or older were eligible for inclusion if they presented with acute symptoms during at least a second recurrence of pericarditis despite treatment with NSAIDs, colchicine and/or glucocorticoids. A pain score of at least 4 on a validated 10-point scale was required, as was a C-reactive protein (CRP) level ≥ 1 mg/dL within seven days of study treatment initiation.
Advertisement
After an initial screening period to confirm trial eligibility, patients underwent a 12-week run-in period in which rilonacept was initiated and background pericarditis medications (NSAIDs, colchicine and prednisone) were tapered and discontinued. Rilonacept was given subcutaneously, initially in a loading dose of 320 mg and then at a weekly dose of 160 mg.
Patients who had a clinical response during run-in (prespecified as a CRP level ≤ 0.5 mg/dL and a weekly average pain score ≤ 2 without a recurrent pericarditis episode) were randomized in a 1:1 ratio to either continued rilonacept (160 mg) or matching placebo, each administered once weekly. The study’s event-driven design specified that this randomized withdrawal period would end upon the observation of 22 adjudicated first recurrence events of pericarditis, with time to first recurrence serving as the study’s primary endpoint.
After closure of this randomized withdrawal period, participants were offered the option of receiving up to 24 months of open-label rilonacept therapy in the study’s long-term extension phase (which remains ongoing).
Of 141 patients assessed for eligibility, 86 were enrolled in the trial’s run-in period, with more than one-third of participants enrolled at Cleveland Clinic. Mean patient age was 44.7 years, and 57% were women. The cause of pericarditis was idiopathic in 85% of patients, with the remaining cases representing post-cardiac injury pericarditis. Roughly half of patients were taking glucocorticoids when they had their qualifying pericarditis episode.
Advertisement
During the trial’s run-in phase, median time to pain resolution or near resolution was 5 days (95% CI, 4-6), and median time to CRP normalization was 7 days (95% CI, 5-8). Manifestations of pericarditis that were present at baseline (pericardial effusion, pericardial rub or ECG changes) resolved by the end of the run-in phase in all but one of the 86 patients.
A total of 61 patients entered the study’s event-driven randomized withdrawal phase. During this phase, pericarditis recurrence occurred in two of 30 patients in the rilonacept group (7%) versus 23 of 31 patients in the placebo group (74%). This translated to a significantly lower risk of recurrence with rilonacept (hazard ratio = 0.04; 95% CI, 0.01-0.18; P < 0.0001). This result was consistent regardless of patients’ baseline use of glucocorticoids.
Notably, no patient who was switched to open-label bailout rilonacept therapy experienced a pericarditis recurrence in the remainder of the randomized withdrawal period.
Secondary efficacy endpoints — maintenance of clinical response, days with minimal or no pain, and percentage of patients with minimal or no pericarditis symptoms — were assessed at week 16 of the randomized withdrawal period. The rilonacept group showed significantly superior outcomes versus the placebo group on all of these outcomes (P < 0.001).
In the trial’s run-in period, four patients (5%) had adverse events that led to study discontinuation. The most common adverse events with rilonacept throughout the study were injection-site reaction and upper respiratory tract infection. The investigators noted that rilonacept’s adverse event profile in the study was consistent with the medication’s FDA-approved labeling for treatment of cryopryin-associated periodic syndromes (CAPS).
Advertisement
“These results demonstrate rapid and sustained reductions in pain and CRP levels, as well as resolution of pericarditis manifestations, with rilonacept therapy,” says Dr. Klein, who served as one of the trial’s two co-principal investigators. “Rilonacept monotherapy reduced the risk of pericarditis recurrence by 96% in this trial, and each of the two recurrence events in the rilonacept arm occurred during temporary interruptions of drug administration.”
“Rilonacept also supported corticosteroid tapering and discontinuation, as all patients on corticosteroid therapy at the start of the study successfully transitioned to rilonacept monotherapy during the run-in period,” adds Cleveland Clinic cardiologist Paul Cremer, MD, who served as a RHAPSODY co-investigator and study co-author.
“This suggests that rilonacept can replace the use of steroids in the future and allow tapering of standard-of-care anti-inflammatories such as NSAIDs, colchicine and prednisone,” says Dr. Klein, noting that each of these therapies has limitations for use in recurrent pericarditis. “IL-1 targeting may be a paradigm shift in treatment of this disease.”
Rilonacept, which is FDA-approved for use in CAPS, received breakthrough therapy designation for recurrent pericarditis from the FDA in 2019 and orphan drug designation for this indication in July 2020. Its developer plans to submit a supplemental biologics license application to the FDA later this year.
RHAPSODY was funded by Kiniksa Pharmaceuticals, which is developing rilonacept for use in recurrent pericarditis.
Advertisement
Advertisement
Why definitive surgical closure is the gold standard, and new ways to make it possible
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon
How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR