A multidisciplinary approach is necessary
By Nikhil Joshi, MD, and Eric Lamarre, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
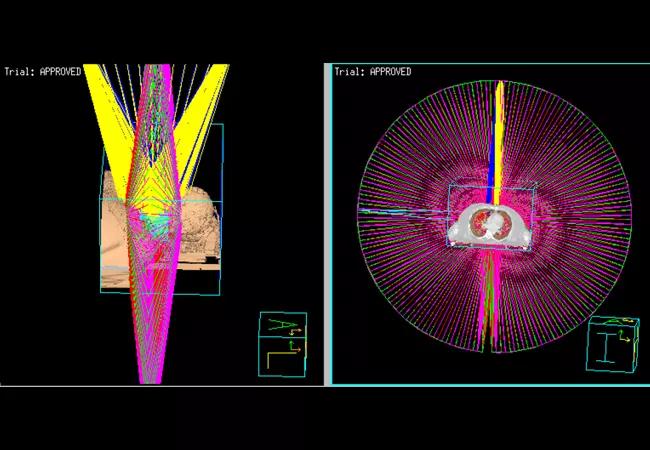
Above image is a ‘rooms-eye view’ of modern VMAT (volumetric arc therapy) utilized for reirradiation showing the arrangement of 5 arcs.
Head and Neck cancer is an important oncologic problem throughout the world. Treatment typically involves some combination of surgery, radiation and chemotherapy, and despite maximal treatment, 30 to 40 percent of cancers will recur locoregionally.1 Additionally, second primary cancers can occur even after the initial cancers are considered cured. In general, these cancers often represent aggressive disease, and their management is particularly challenging especially for those recurring in the face of previous radiation.
Patients with recurrent or second primary head and neck cancers have several treatment options, ranging from palliation to aggressive surgery and reirradiation. Each treatment is associated with variable acute and late toxicity; appropriate treatment selection individualized to the patient is critical. Older studies of either reirradiation with chemotherapy2 or surgery followed by reirradiation with chemotherapy3 are indicative of modest oncologic outcomes in the face of severe toxicity. Patients in these studies included both new primaries and recurrent cancers. Surgical and radiation techniques employed were also older or outdated by modern standards. Better patient selection and the use of modern radiation and surgical techniques can potentially improve the therapeutic ratio leading to better outcomes.
Recent efforts led by Cleveland Clinic and others (a multi-institution cohort study, or the MIRI/multi-institution reirradiation collaborative) have shed light on optimal patient selection for reirradiation in the modern era. A recursive partitioning analysis indicated that patients with a recurrence or second primary cancer more than two years after their first course of radiation and undergoing surgery did best with adjuvant reirradiation. This group of patients had a two-year survival of 61.9 percent. Patients who could not undergo resection, or those with a recurrence/second primary less than two years from radiation but with no organ dysfunction, had an intermediate outcome (two-year survival of 40 percent). Finally, patients with a recurrence or second primary cancer less than two years after radiation or with organ dysfunction did the worst, with reirradiation resulting in a two-year survival of 16.8 percent.4 Therefore, aggressive treatment may be pursued for the first and second group, while avoiding overtly aggressive treatment for the third group.
Advertisement
Apart from oncologic outcomes, toxicity is a major concern with reirradiation. Older studies indicate grade 3 and grade 4 toxicity of 39 percent and a grade 5 toxicity (death) of 7 percent3 with conventional reirradiation. More modern experience with reirradiation using advanced treatment planning (IMRT and particularly VMAT) is associated with lower toxicity (>/= grade 3 toxicity of 14.2 percent and grade 5 toxicity of 1.2 percent in the acute setting).4 Modern reirradiation using advanced treatment planning and guided by better patient selection has led to better oncologic and toxicity outcomes.
The improvements seen in reirradiation have occurred alongside similar improvements in resection and reconstructive techniques over the last few decades. When surgery is necessary after definitive chemoradiation therapy, vascularized tissue transfer has become the standard practice employed. This provides tissue that has not been previously radiated to a field that has been treated and is at increased risk of wound healing related issues and increased fibrosis. The vascularized tissue helps to optimize healing and improves the functional outcomes of patients when a radical resection is necessary for tumor control.
The following case vignette demonstrates the utilization of modern surgery and reirradiation for a second primary cancer that developed after previous radiation.
A 63-year-old gentleman with a previous history of stage III squamous cell carcinoma of the supraglottic larynx treated with definitive chemoradiation at an outside facility presented with a second primary cancer in the glottis 10 years later.
Advertisement
He presented with increasing shortness of breath and hoarseness. A direct laryngoscopy revealed a glottic primary. Biopsy was positive for squamous cell carcinoma, and imaging was suggestive of recurrent T4aN1M0, stage IVA cancer. He had minimal late toxicity from previous radiation and was otherwise medically fit. A decision was made to proceed with primary surgical resection and reconstruction followed by adjuvant chemoradiation, keeping in mind his previous history of radiation and current extent of disease. He underwent a total laryngopharyngectomy with nodal dissection and reconstruction with an anterolateral thigh free-flap using microvascular reconstruction. Pathology was notable for a 3.8 cm primary cancer invading the thyroid lamina with extensive lymphovascular space involvement, along with 4 out of 59 nodes positive for disease. The final stage was rpT4aN2bM0, stage IVA.
He then underwent reirradiation to a dose of 58 Gy in 29 fractions with one cycle of bolus cisplatin. The radiation was delivered with volumetric modulated arc therapy using five non-coplanar arcs (figure 1). One fraction was dropped for increased inhomogeneity in the radiation plan as can be expected with reirradiation (isodose lines depicted in figure 2 with dose-volume histogram in figure 3). The second cycle of chemotherapy was deferred due to the patient’s wishes. He had a percutaneous gastrostomy (PEG tube) for feeding through treatment. He tolerated treatment with grade 2 mucositis, dermatitis and taste changes along with grade 1 xerostomia, pain and weight loss. At the three-month follow-up, he was eating most solids and his taste continues to improve without requiring a PEG tube. He has grade 2 skin/soft tissue fibrosis. Clinical examination and imaging did not reveal any evidence of disease.
Advertisement
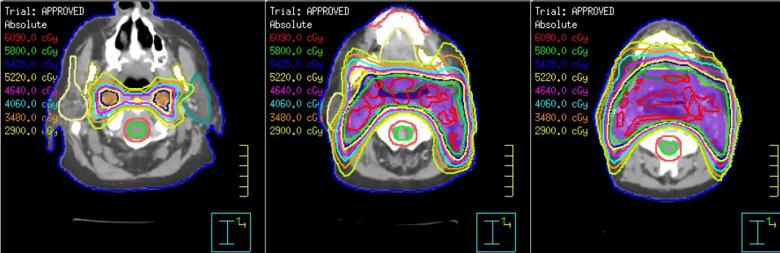
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d6e7462c-c3b6-4f89-b4dc-a76fbf16e36d/Joshi-Image-2_png)
Reirradiation plan demonstrating various isodose lines and target in purple covered by the 58 Gy isodose line. Notice the inhomogeneity depicted by the 6090 cGy isodose line in red
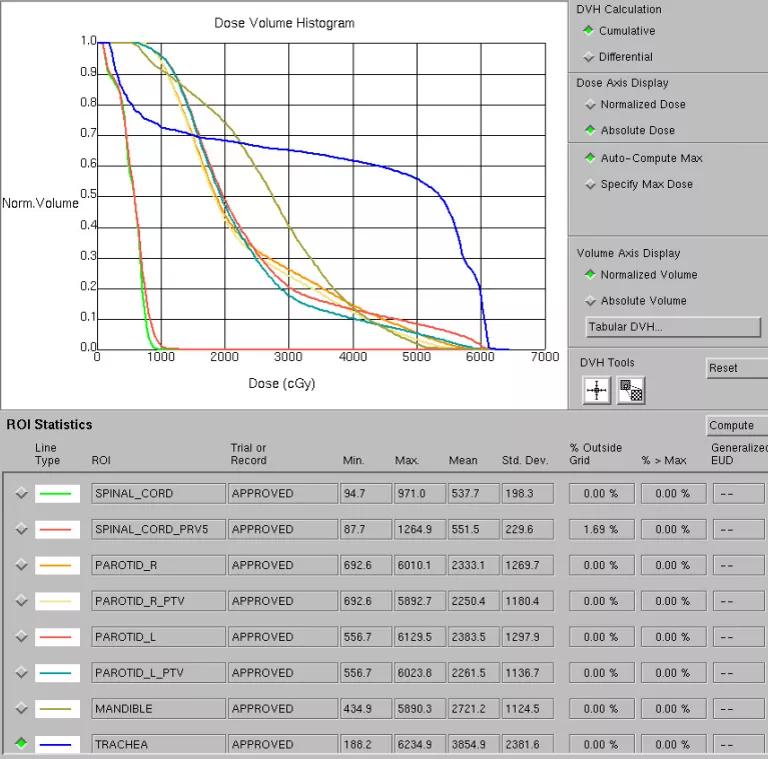
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/04953c9a-20f1-4680-9a54-70555a720e08/Joshi-Image-3_png)
Dose-volume histogram (DVH) demonstrating optimal sparing of structures at risk especially the spinal cord (maximum dose < 10 Gy)
Dr. Joshi is on staff of Cleveland Clinic’s Radiation Oncology Department and Dr. Lamarre is a surgeon in the Head & Neck Institute.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors