A comparison with cautery/laser

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/48cc8ab6-a9a9-4dba-96c0-a242ceffb618/21-HNI-2078916-SclerotherapyTreatment-HHT-Woodard-CQD-hero_650x450_jpg)
Sclerotherapy
Sodium tetradecyl sclerotherapy (STS) achieves epistaxis control with fewer procedures and postoperative complications than electrocautery and/or laser photocoagulation (C ± L) in patients with hereditary hemorrhagic telanglectasia (HHT), according to a Cleveland Clinic study recently published in Laryngoscope. The study is the first to quantify the number of procedures that patients with moderate to severe HHT require for control of mild epistaxis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“It’s terribly common in HHT patients, and while we have treatments, patients often need them multiple times, which risks thermal injury to surrounding mucosal tissue, or progression to effective surgical approaches that unfortunately cause their own slate of problems,” says Troy Woodard, MD, staff in Cleveland Clinic’s Head & Neck Institute and lead author of the study. “STS controls epistaxis better and with less risk to patients than our current methods, and we should consider it first among surgical interventions for these patients.”
The most common surgical approach to moderate to severe epistaxis is bipolar electrocautery and laser photocoagulation. Less common, STS involves injection of telangiectasias to induce sclerosis and vessel wall collapse and has been proven safe and effective in reducing epistaxis severity score [ESS] in HHT. For refractory cases, septal dermoplasty and Young’s procedure for complete nasal closure are effective but rife with postoperative complications.
In this retrospective analysis, researchers assessed 67 patients with HHT and moderate to severe epistaxis (ESS > 4) who were treate with either C ± L (N = 34) or STS (N = 33) and had available follow-up data through 24 months. Less than one-third (27%) of patients in the STS group had undergone a prior C ± L. Patients who had undergone septal dermoplasty, arterial embolization, young’s procedure and submucosal bevacizumab injection, as well as patients who had been evaluated while on systemic anti-angiogenic therapies.
Advertisement
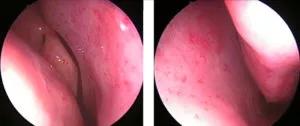
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a66c3402-6238-4f4a-a730-ad6a1d5c1a63/21-HNI-2078916-SclerotherapyTreatment-HHT-Woodard-CQD-inset1_800x337-300x126_jpg)
Endoscopic view of nasal HHT Teleangiectasia
“As a tertiary referral center and an HHT Foundation-designated HHT Center of Excellence, we see patients from across the country,” says Joseph Parambil, MD, staff in the Respiratory Institute at Cleveland Clinic. “That uniquely situates us to draw from a large group of patients who have undergone a range of procedures under the care of our HHT experts.”
The research team’s primary focus was the number of procedures required to keep ESS in the mild range. They also assessed differences in postoperative complications, iron stores, hemogloblin levels, hematologic support and quality of life (QoL) scores.
The team’s analysis demonstrated a significant difference in the number of STS procedures (1.6, range 1-4) required to maintain a mild ESS in comparison with C ± L (3.6, range 1-8) (P = 0.003). STS also significantly reduced septal perforation (3% vs. 29%, P = 0.006), nasal crusting (3% vs. 29%, P = 0.001) and foul odor (3% vs 35%, P < 0.001), common complications of surgical approaches to epistaxis. No differences were seen in hematologic support, iron stores, hemoglobin levels or QoL scores.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/48eeb806-3bfa-4df2-bbba-5d907bbc918a/21-HNI-2078916-SclerotherapyTreatment-HHT-Woodard-CQD-inset2_800x664-300x249_jpg)
Submucosal injections of sodium tetrdecyl sulfate (STS)
“Our most important finding was the reduction in septal perforations, which disrupt airflow and cause more mucosal drying and nasal crusting, which makes epistaxis worse,” says Dr. Woodard. “That’s part of the reason STS reduces the need for repeat interventions. It’s not exacerbating the problem it’s trying to fix.”
Advertisement
Recent studies have shown promise in the systemic and topical administration of anti-angiogenics, and experts are hopeful that the combination of better medical and surgical treatments can reduce the morbidity and mortality associated with epistaxis in patients with HHT.
“We are coming closer to defining a standard of care for moderate to severe epistaxis,” says Dr. Woodard, “and our results support the role of STS in that standard.”
Advertisement
Advertisement
Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor
Case study illustrates the potential of a dual-subspecialist approach
Evidence-based recommendations for balancing cancer control with quality of life
Study shows no negative impact for individuals with better contralateral ear performance
HNS device offers new solution for those struggling with CPAP
Patient with cerebral palsy undergoes life-saving tumor resection
Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition
Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.