Nathalia Velasquez, MD, is the Co-Director of the Endoscopic Skull Base and Pituitary Surgery Center at Cleveland Clinic Weston Hospital. As a fellowship-trained skull base surgeon and rhinologist, Dr. Velasquez is part of a multidisciplinary team caring for patients with benign and malignant skull base tumors.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
She is also a self-professed “nosekeeper.”
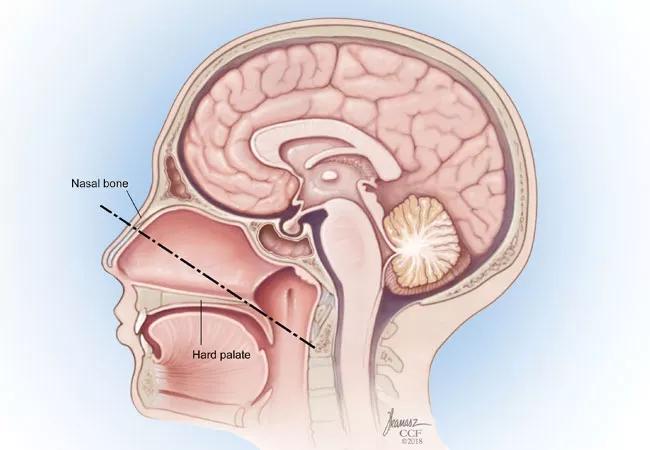
Endoscopic skull base surgery (ESBS) uses a natural corridor through the nose to manage skull base lesions, causing less tissue trauma and a faster recovery. It has gained popularity over the past two decades for the management of a wide range of intranasal and skull base pathologies.
“Better anatomical understanding of the region and advances in instrumentation, neuronavigation, and improved surgical techniques have broadened the scope of transnasal surgery,” says Dr. Velasquez. “Endoscopic endonasal surgery provides a safe and effective surgical option, in many ways surpassing microsurgical transsphenoidal approaches, which were the gold standard for decades.”
For example, technology advancements have achieved a panoramic view during endoscopic endonasal surgery that improves tumor resection, notably for macroadenomas with extrasellar extension. “Patients also enjoy a faster postoperative recovery, with less pain and no external scarring,” she says.
At Cleveland Clinic Weston Hospital, ESBS is used to access the anterior, sellar, and in some cases the lateral areas of the cranial base. Most pituitary adenomas are endoscopically resected as are many other types of skull base tumors, including chordoma, chondrosarcoma, intraventricular tumors and cysts, tumors in the orbital apex, tuberculum sellae meningioma and olfactory groove meningioma, and trigeminal schwannomas.
Endoscopic endonasal procedures for skull base lesions require close collaboration between a neurosurgeon and a rhinologist. Dr. Velasquez and her colleague Hamid Borghei-Razavi, MD use a simultaneous two-surgeon binarial approach to tackle a wide array of complex cranial conditions.
Advertisement
“The delicate structures involved in this type of surgery require multiple hands working simultaneously,” says Dr. Velasquez. “My role is to create a safe operative corridor and to achieve optimal reconstruction following tumor resection.”
Dr. Velasquez also is responsible for following patients after surgery to minimize postoperative complications and maximize nasal function. Potential complications include diabetes insipidus, cerebrospinal fluid (CSF) leak, and meningitis, as well as chronic rhinosinusitis, empty nose syndrome, and smell disorders.
“That’s why I consider myself the nosekeeper,” she says. “My goal is to have patients return to a normal quality of life after all the healing is complete.”
The expanded indications for endoscopic endonasal surgery for larger and more complicated lesions has led to improved reconstructive techniques for managing larger skull base defects. This reduces the risk of postoperative CSF leaks, which can put patients at risk of significant complications, including meningitis and pneumocephalus.
Cleveland Clinic’s surgical teams in Florida and Ohio use a reconstructive ladder that progresses from synthetic grafts and local tissue (free or pedicled) flaps through extranasal vascularized flaps and free tissue transfer from distant sites. These include single-layer or multilayer repairs.
“While the nasoseptal flap continues to be the workhorse of intranasal reconstruction, we have many approaches that allow us to tailor the surgical repair based the size and complexity of the defect, the pathology being treated, the presence of a CSF leak, and the patient’s history of previous radiation or surgery,” explains Dr. Velasquez.
Advertisement
She and Dr. Borghei-Razavi also participated in a research study that found obesity to be a major risk factor in developing CSF leaks for patients who undergo endoscopic endonasal surgery for posterior fossa skull base tumors. “This further reinforces the need to look at a patient holistically when determining the best reconstructive approach.”
In addition to high-tech innovations that have advanced ESBS over the years, the recent development of a low-tech device also has improved this surgical approach. Approved by the FDA in 2018, the nasal access guide (NAG) is an anatomically-shaped, stretchable, and watertight stent designed to minimize iatrogenic tissue trauma and improve visualization and workflow during procedures. The NAG is placed in the bilateral nares to provide a working corridor to the posterior nasal cavity.
Prior to joining Cleveland Clinic, Dr. Velasquez was part of a research team that evaluated the use of the NAG and its impact on operative workflow and clinical outcomes. Their findings were published in the Journal of Neurological Surgery.
“We found the device to be very effective in reducing instances of inadequate visualization and creating greater efficiency by reducing the number of instrument passes needed during a procedure,” she says. “But one of the greatest advantages of the nasal sleeve is the ability to protect patients from unnecessary mucosal trauma, which can delay healing and may result in additional crusting, synechiae, and septal perforation.”
Advertisement
Dr. Velasquez now uses the device for all endoscopic endonasal surgeries. “It goes back to protecting my patients, that’s my bottom line,” she adds.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.