Stratified sperm count and motility data informs IVF decision-making

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0ccc75dd-832e-459a-a5cf-04efe67449e5/650x450-Andrology_jpg)
Sperm motility
For males with severe oligospermia (low sperm counts) or azoospermia (where sperm is surgically extracted from the epididymis or the testis), identifying sperm characteristics that are associated with a successful live birth after IVF/ICSI would be useful for patient counseling.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A recent study by Cleveland Clinic fertility specialists establishes that an objective grading scale for assessment of severely compromised sperm specimens can predict the likelihood of achieving successful pregnancy after intracytoplasmic sperm injection (ICSI) during in vitro fertilization (IVF) treatment.
The study focused on cases of severe oligospermia (OS) or azoospermia. It retrospectively analyzed 243 ICSI cycles using epididymal sperm (ES), testicular sperm (TS) and sperm from men who have fewer than one million sperm per milliliter. Sperm assessments were made prior to the IVF consult and initiation of the IVF cycle.
A systematic approach to this assessment had to be developed, since samples with low counts under 0.1 million/ml could not be quantitated using standard counting chambers. IVF cycle data was stratified into four groups by severity of sperm count and further analyzed by quality of motility.
Group 1: 0.1 to 1 million motile sperm/ml
Group 2: Five µl drop: At least 1 or more motile sperm observed per high-powered field
Group 3: Five µl drop: At least 1 or more motile sperm in entire drop
Group 4: Twenty µl drop: At least 1 or more motile sperm per 20-microliter drop.
Within each group, quality also was assessed and graded:
A: forward motility
B: distinct twitching or movement in place
C: slight sway
D: non-motile
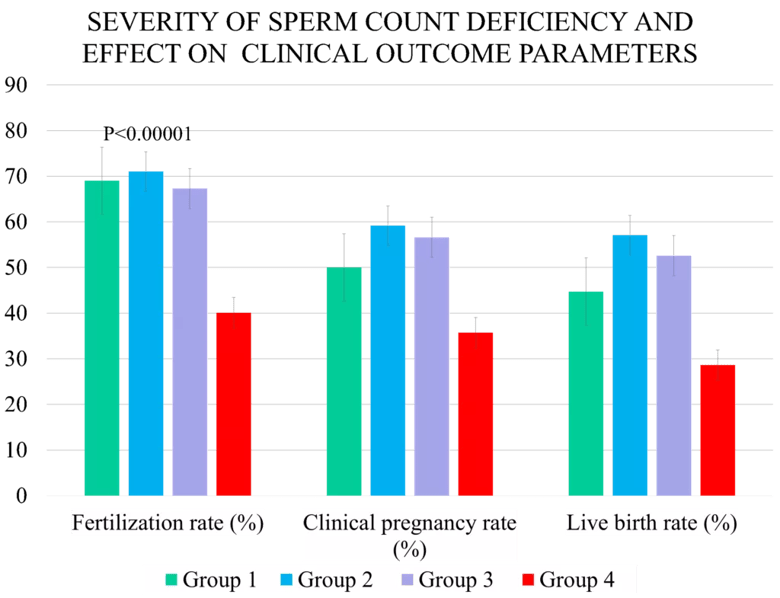
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5397bb6a-6573-4229-8e7b-f7276480c5a2/Desair-chart-1024x785_png)
ICSI cycles using Group 4 sperm had the lowest fertilization rates – only 40.1%, compared to 69%, 71% and 67.3% for groups 1 through 3, respectively. The live birth rate for Group 4 was 28.6%, compared to 44.7%, 57.1% and 52.6% for groups 1 through 3.
Advertisement
Non-motility also was a strong predictor of lower fertilization rates. Grade D sperm fertilization was 42.5%, compared to 68.8%, 60.5% and 63.6% for grades A-C, respectively.
Although the outcomes might seem predictable, Nina Desai, PhD, HCLD, Director of Cleveland Clinic’s IVF/Andrology Laboratories, says the study underscores the value of pre-ICSI assessment to improve strategies and manage patient expectations.
“This is a system I developed because it was very frustrating not having a clear picture of whether there would be sufficient quality of sperm in a frozen sample to achieve a good outcome,” says Dr. Desai. “With severe male factor cases, systematic assessment of sperm allows me to make better recommendations to the doctors and to staff the lab appropriately for difficult cases that will take hours of searching for sperm.”
Managing patient expectations and proper counseling about sperm quality is important when dealing with severe male infertility, says Dr. Desai. “What is the likelihood that we’ll get fertilization and a live birth is a frequently asked question.”
The other logistical question is whether to use fresh or frozen sperm. Men who are oligiospermic can produce samples that vary from one ejaculate to another.
“They may have a few sperm on one collection, but on the day of the retrieval, they may potentially have nothing. For this reason, whenever possible we ask them to bank several times,” she says. “Then we make an assessment based on the post-thaw as to whether we think we should proceed forward or not.”
Advertisement
The freezing process can degrade sperm quality, says Dr. Desai. “Where you might find one sperm in five high powered fields with a fresh sample, you might find one in 10 with a frozen.”
So if a post-thaw frozen sample isn’t good, the patient needs to be counseled about the odds of success using a fresh sample. “There’s a chance that they may have no sperm to fertilize the eggs,” she says.
Sperm also can be harvested through tissue biopsy of the epididymis or testis.
“It’s very hard to coordinate the woman’s egg stimulation cycle and a sperm extraction procedure for the male, since both surgeries have to occur on the same day. For this reason, in most cases we rely on using frozen sperm for the ICSI,” she says.
Cleveland Clinic’s laboratories specialize in male factor fertility.
“Unlike other laboratories, when we have a severe male-factor case, I might put two embryologists on it to look for sperm,” she says. “If two embryologists look for three hours for sperm, that’s six man hours of searching. Many labs don’t have the ability to do that.”
That investment of resources especially pays off in the most challenging male-factor fertility cases. In 2011, a couple being treated at Cleveland Clinic Fertility Center made national news when they gave birth to a healthy baby girl after undergoing ICSI using a single sperm cell that had been frozen using a technique developed by Dr. Desai. “We can get really good pregnancy and live birth rates even when we’re working with as little as one sperm in five microliters,” she say. “That’s such a low number, and yet we can still do quite well. It just means the hours that the laboratory spends will be longer.”
Advertisement
But for any case, the assessment process provides valuable information. “It allows me to convey to the doctors the severity of the male-factor fertility issues, and therefore helps doctors convey to patients what their likelihood of success will be with the frozen specimen,” says Dr. Desai.
“It also helps us to decide how to proceed. If a frozen specimen is really poor, the doctor may suggest another testicular biopsy with a fresh sample,” she adds. “They may want to discuss egg freezing or having donor sperm as a backup. Patients hear about fantastic pregnancy rates for our fertility program, but it’s also important that they understand that it all starts with having something to work with.”
It also helps for laboratory scheduling, she adds.
“Lab staffing becomes really important when you’re orchestrating work around these cases,” says Dr. Desai. “If we know there’s a very severe male factor case coming through, I will staff the lab accordingly. If there’s a very severe case and we need more hands, then I’ll have more hands available.”
The study was presented at the American Society for Reproductive Medicine’s 2021 Annual conference.
Advertisement
Advertisement
Multidisciplinary teams work together in in-situ scenarios
Uterine transposition cleared the field for radiation therapy
ACOG-informed guidance considers mothers and babies
Prolapse surgery need not automatically mean hysterectomy
Artesunate ointment shows promise as a non-surgical alternative
New guidelines update recommendations
Two blood tests improve risk in assessment after ovarian ultrasound
Recent research underscores association between BV and sexual activity