Study evaluates stiffness distribution using Brillouin microscopy
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Corneal ectasia is a rare but serious complication that can occur after laser in situ keratomileusis (LASIK), leading to progressive corneal thinning and steepening with induced irregular astigmatism and vision loss. Corneal cross-linking (CXL) halts corneal ectasia progression and has been approved for use by the U.S. Food and Drug Administration since 2016. The approved standard (or Dresden) CXL protocol (S-CXL) includes epithelium removal, riboflavin soaking on the corneal surface over the LASIK flap, followed by ultraviolet light (UVA) irradiation. The majority of risks associated with S-CXL, including corneal ulceration or scarring, arise from epithelial removal.
Performing CXL under the LASIK flap (flap-CXL) has been proposed to stabilize post-LASIK ectasia. Instead of performing corneal debridement, as in S-CXL, the existing flap is reflected, with riboflavin applied directly onto the stromal bed followed by flap repositioning and UVA irradiation. This flap-CXL technique, if effective, could mitigate most of the complications associated with S-CXL, improve patient comfort and speed patient recovery. This technique, however, bears similarities to prophylactic CXL at the time of primary LASIK (LASIK Xtra), which has been shown to have limited biomechanical impact.
Our group recently evaluated the depth-dependent stiffness distribution of CXL performed over the flap (S-CXL) or under the flap (flap-CXL) in a laboratory model (porcine eyes) using Brillouin microscopy.
Advertisement
Brillouin optical microscopy is a novel technique based on Brillouin light-scattering spectroscopy for probing the viscoelastic properties of a sample with three-dimensional resolution in vivo and without tissue contact. Spontaneous Brillouin light scattering arises from the interaction of photons and acoustic phonons, through propagation of thermodynamic fluctuations, in a sample. The resulting frequency shift and the line width of the Brillouin spectrum are related to the longitudinal viscoelastic modulus, which in turn is related to the conventional Young’s (or shear) moduli through a log–log linear relationship.
The custom-built device in our laboratory measured the optical frequency shift using a Brillouin spectrometer after using a continuous-wave laser as the probing light. The scattered light, collected by the same objective lens, was coupled into the Brillouin spectrometer and captured by an electron multiplying charge-coupled device (EMCCD) camera.
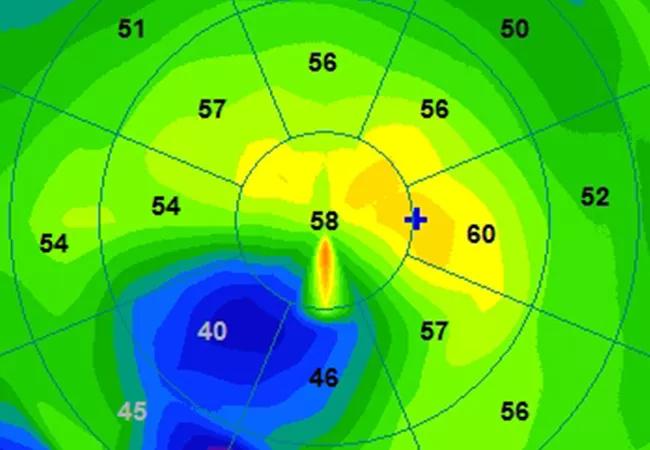
Depth-dependent Brillouin results showed that flap-CXL achieved only 50% of the stiffening effect of S-CXL in the anterior third of the cornea, the region where the majority of the CXL effect is seen (Figure 1).
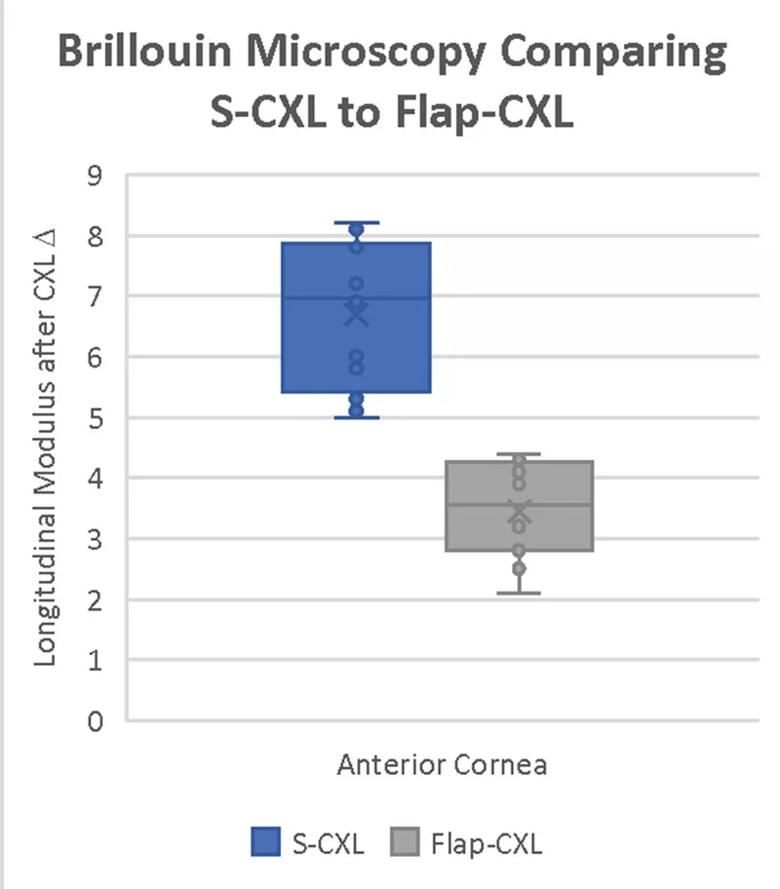
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1a6bdaad-7123-4afd-855b-57ebc761d771/21-EYE-2084161-CQD-Brillouin-Analysis-Inset-1_jpg)
Figure 1. This plot shows the relative difference after CXL for both S-CXL and flap-CXL groups in the anterior third of the cornea. There was significantly greater stiffening induced in the S-CXL samples.
In the middle and posterior regions, there were no significant differences between techniques. These results were confirmed with direct mechanical stress-strain testing (Figure 2).
Advertisement
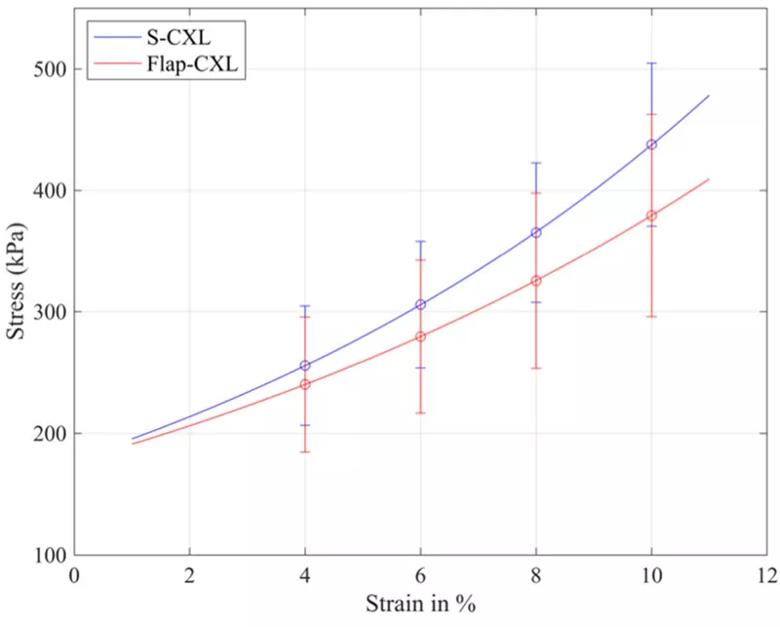
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0f68bffd-cb67-435a-8b97-6c233486bbcc/21-EYE-2084161-CQD-Brillouin-Analysis-Inset-2_jpg)
Figure 2. This plot shows the stress-strain curves fitted by mean values at strains of 4%, 6%, 8% and 10%. S-CXL induced greater stiffening than flap-CXL at all selected strains.
At this time, based on these results, we do not recommend modifications to the standard protocol CXL for postoperative ectasia, as there was a significant reduction in efficacy with the flap-CXL technique in this model. Future studies will evaluate the efficacy of CXL protocols in human trials supported by Research Project Grant (R01) funding from the National Institutes of Health (ClinicalTrials.gov identifier: NCT04598932).
Dr. Randleman is a specialist in corneal and intraocular refractive surgery at Cole Eye Institute.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift