First five-year prospective study provides valuable data to guide decision-making

Surgical treatments for idiopathic subglottic stenosis (iSGS) vary greatly in effectiveness and reoperation rates. That is the major finding of a five-year follow-up study comparing surgical procedures, conducted by the North American Airway Collaborative (NoAAC). Cleveland Clinic is an active member of the group and has one of the largest populations of iSGS patients.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This is a landmark study that provides valuable data on treating a rare disease that has not been adequately studied,” says William Tierney, MD, study-co-author and a laryngologist at the Cleveland Clinic Head and Neck Institute.
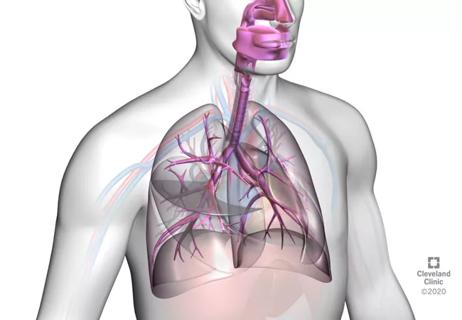
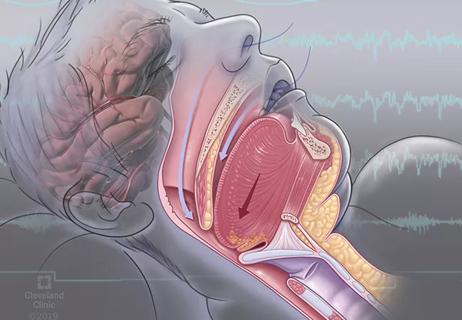
Affecting about one in 400,000 people, mostly Caucasian women, idiopathic subglottic stenosis is an fibroinflammatory disease characterized by recurrent upper airway narrowing which causes symptoms such as shortness of breath, chronic coughing and hoarseness. iSGS requires intervention to maintain ventilation and often recurs, requiring repeat treatments. It is treated with steroid injections (medical therapy) at an early stage and surgery when more advanced.
Three surgical techniques are commonly used to enlarge the upper airway: endoscopic dilation (ED), which stretches the windpipe with a balloon or surgical instrument; endoscopic resection with adjuvant medical therapy (ERMT) which removes scar tissue from the windpipe; and cricotracheal resection (CTR), open surgery that removes scarred tissue and reconstructs the narrowed areas of the trachea and windpipe.
“This is a condition that requires a high level of expertise. If a patient is struggling with shortness of breath with no explanation, they should be referred to a specialist to determine if there is a stenosis,” says Dr. Tierney.
NoAAC first conducted a prospective three-year study comparing ED, ERMT and CTR. The study cohort included 810 patients (798 female and 787 white, with a median age of 50 years) who were untreated, newly diagnosed or previously treated for iSGS. The majority of patients were treated with ED (603, 74.4%), followed by ERMT (121, 14.9%) and CTR (86, 10.6%).
Advertisement
Over the course of the three-year study, 185 patients (22.8%) had a recurrent surgical procedure with major differences by modality: CTR, one patient (1.2%); ERMT, 15 (12.4%); and ED, 169 (28.0%).
Patient quality-of-life was evaluated using the Clinical COPD (chronic obstructive pulmonary disease) Questionnaire (CCQ), Voice Handicap Index-10 (VHI-10) and the 12-Item Short-Form Health Survey (SF-12v2).
Overall, CTR was the most durable treatment but showed the greatest perioperative risk and the worst long-term voice outcomes. ERMT was associated with better disease control than ED and had minimal impact on vocal function.
NoAAC followed up the initial study with a five-year update using the same protocol. Of the original 810 patients, 487 agreed to participate: 58% (351/603) of the ED group, 78% (94/121) of the ERMT group and 49% (42/86) of the CTR group.
During the five-year study period, 204 patients (42%) had a recurrent operation; consistent with the three-year report, it differed by modality: CTR had a 5% recurrence rate (2/42), followed by 30% for ERMT (28/94), and 50% for ED (174/351).
Patient quality of life and voice function were evaluated using the SF-12v2 and VHI-10. ED had lower quality-of-life scores than CTR and ERMT which had comparable scores. Regarding voice function, ERMT was again superior to CTR.
“This is the first study to report five-year prospective data for this disease. We now have definite data to present to patients. Knowing the percentage of patients who will have a recurrence will help us to make more informed clinical decisions,” says Dr. Tierney.
Advertisement
The study appears in Otolaryngology – Head and Neck Surgery.
NoAAC will be conducting a prospective study to assess outcomes of office treatment with steroids.
Advertisement
Advertisement
First retrospective study compares balloon and rigid bronchoplasty

A new study indicates high patient satisfaction with the Maddern Procedure, but the technique can be technically challenging for surgeons

Recent breakthroughs have brought attention to a previously overlooked condition

Case study illustrates the potential of a dual-subspecialist approach

Findings show profound muscle loss variance between men and women
New tools and protocols to improve care

Endoscopic balloon dilation during pregnancy helps optimize outcomes
For the first time, risk is shown after accounting for underlying contributions of pulmonary disease