A new study indicates high patient satisfaction with the Maddern Procedure, but the technique can be technically challenging for surgeons
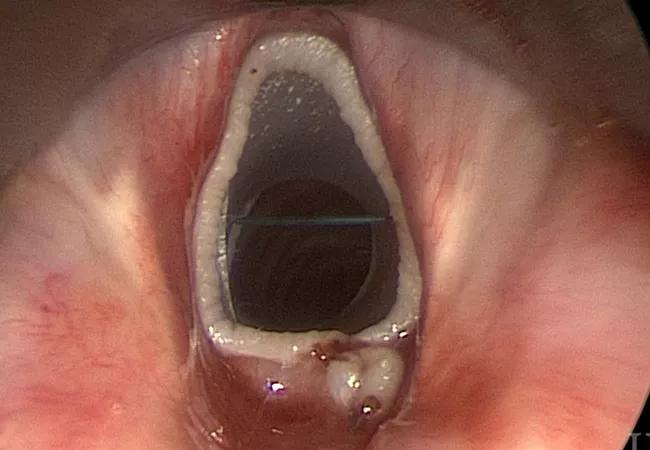
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b22885f8-2399-4dff-8607-934192e945ac/22-HNI-2986779-CQD-Hero-650x450-1_jpg)
Maddern Procedure
A surgical advance called the “Maddern procedure” offers patients with refractory subglottic stenosis a voice quality-preserving alternative to a maximally invasive resection.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Robert Lorenz, MD, of Cleveland Clinic’s Head and Neck Institute, learned the procedure from its originator, Dr. Guri Sandhu, of Imperial College London, and brought it to the United States in 2015. The technique has since been adopted in several other U.S. academic centers, but Cleveland Clinic maintains the largest patient volume to date.
Subglottic stenosis, a narrowing of the intraluminal airway below the glottis due to scar tissue, occurs in about 1 in 400,000 people. Of the three types – iatrogenic, autoimmune or idiopathic – the latter occurs almost exclusively in women.
First-line treatment is minimally invasive, aimed at maintaining a patent airway to facilitate airflow. Options include endoscopic steroid injections directly into the stenosis, mitomycin-C application, laser resection, and dilatation. However, over time, patients often become refractory to endoscopic treatment.
Until now, the usual next step has been open cricotracheal resection. While often curative of the stenosis, this procedure can result in loss of anterior cricoid cartilage and the cricothyroid muscle’s function of elongation and shortening of the vocal cord. Subsequent changes in the patient’s vocal frequency and pitch variation can occur.
The Maddern procedure is a new alternative for patients to try before moving on to a maximally invasive resection procedure. “We’re excited about that because these are all females and resection affects their voices long-term. The Maddern procedure does not because it doesn’t remove that part of the airway,” Dr. Lorenz says.
Advertisement
The technique, named after the first patient to undergo it, involves subepithelial resection and relining of the subglottis with an autologous skin graft. A soft-tissue shaver is used to remove the subglottic scar down to the cartilage, a temporary silicone stent is fitted and the graft is stitched around it. The stent is left in for two weeks to allow for attachment of the graft, then removed. During that time, the patient is discharged from the hospital but remains nearby for monitoring.
In a recently published paper, Dr. Lorenz describes the Cleveland Clinic team’s experience, including modifications made along the way and outcomes, with the first 28 patients to undergo the procedure beginning in 2015. The patients included five with granulomatosis with polyangiitis as the cause of their subglottic stenosis, while the other 23 were idiopathic. All 28 were female.
Lorenz performed the procedure transcervically in the first two patients, then switched to a transoral approach for the other 26. “I had originally thought you had to approach the subglottis from below, from the tracheal side. But then Dr. Sandu encouraged me to perform it trans-orally, so I exclusively use that approach now,” he says.
Another lesson was that, contrary to initial belief, the best candidates were those with high subglottic stenosis, rather than low disease at the bottom of the cricoid and close to the trachea. “As it turned out, the patients who didn’t have long-term airway improvement were the ones with low disease. The trachea is not a great place to attempt a Maddern procedure,” Dr. Lorenz says. “On the other hand, those with the stenosis higher up tolerated the stent in the graft very well, and their treatment was more often curative.”
Advertisement
The source of the graft was another major change. For the first 20 patients, Dr. Lorenz used a split-thickness graft from the thigh. While that provided reliable material, over time the keratin within it would accumulate in the patients’ airways and cause discomfort. That material was lasered out in 13 patients, meaning they had to return for another procedure.
Dr. Lorenz began using buccal grafts instead. That tissue is softer and more challenging to work with due to its consistency, but the long-term results are superior given the lack of post-op keratin build-up. He is currently exploring use of even better materials, such as umbilical cord or pluripotent cells.
Of the 28 total patients, 19 (73%) appeared to achieve favorable outcomes, while an additional four (14%) had their tracheal narrowing successfully treated with subsequent therapy, including cricotracheal resection in two, for an overall 88% success rate.
There were no intraoperative or postoperative complications, and all patients tolerated the stent for two weeks. About a third of the patients reported cough and production of phlegm following the procedure.
More than 80% reported having no problems with their voices, and 24 of 28 gave a score of 7 or higher when asked if the procedure improved their quality of breathing. Asked if they would undergo the procedure again knowing what they know now, 26 said “yes” while the only two who said “no” were the ones who underwent subsequent cricotracheal resection.
“This study demonstrates that not only can stenting and relining of the subglottis be done safely without perioperative complications, but long-term patency in most patients, for at least six years now, can be achieved,” Lorenz says.
Advertisement
However, he adds, “Because it’s a technically challenging procedure, volume does matter. You want to go to a place that does this a lot.”
More insight from Dr. Lorenz:
Evolution and Outcomes of Subglottic Stenosis and the Maddern Procedure Part I (Podcast)
Evolution and Outcomes of Subglottic Stenosis and the Maddern Procedure Part II (Podcast)
Advertisement
Advertisement
First five-year prospective study provides valuable data to guide decision-making
First retrospective study compares balloon and rigid bronchoplasty
Recent breakthroughs have brought attention to a previously overlooked condition
Case study illustrates the potential of a dual-subspecialist approach
Findings show profound muscle loss variance between men and women
New tools and protocols to improve care
Endoscopic balloon dilation during pregnancy helps optimize outcomes
For the first time, risk is shown after accounting for underlying contributions of pulmonary disease