Researchers develop first-of-its-kind neoantigen atlas to better understand immunotherapy resistance
Immunotherapy has come to the forefront of cancer treatment, yet an estimated half of all patients do not respond to this therapy. Researchers at Cleveland Clinic led a team in investigating this phenomenon. “Understanding why the immune system responds in some cases and not others is of great interest because this may help overcome resistance,” explains Tyler Alban, PhD, co-first author of the study and a computational biologist and faculty member at Cleveland Clinic.
Patients who responded had a notable reduction in mutational burden after starting immunotherapy. However, the researchers were surprised to find that patients who did not respond to immunotherapy also had a neoantigen response. The study results, which were published in Nature Medicine, showed that in the latter cases, the immune system recognized subclonal neoantigens as opposed to responders who recognized clonal neoantigens. “These findings give us hope that if we can modify their antigen response, we might be able to get their immune system to better recognize [and attack the cancer cells],” says Alban.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As cells mutate into cancer, small peptides called neoantigens are produced. The immune system is constantly surveilling for these neoantigens, which can then be specifically targeted by the immune system. Understanding the mechanisms of immunotherapy response and resistance is a highly researched area. “There’s enormous potential for improving immunotherapies if we knew what those targets and processes were,” explains Timothy Chan, MD, PhD, study co-author and Chair of Cleveland Clinic's Global Center for Immunotherapy.
“Only about 3-10% of mutations are seen by the immune system, so it’s very important to be able to predict and identify what those are,” explains Dr. Chan. “The only way to do so is to painstakingly go through and identify large volumes of neoantigens and figure out what characteristics allow the immune system to preferentially target them.”
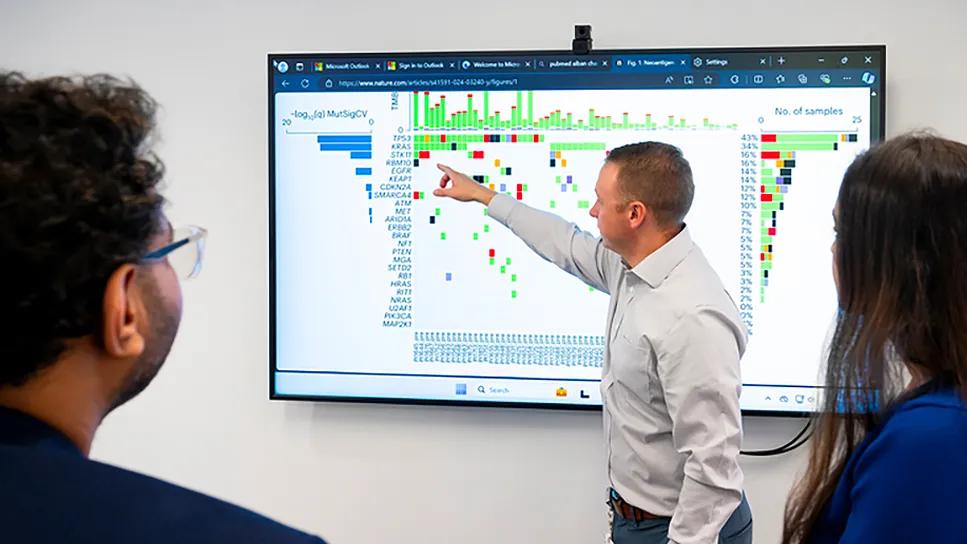
To help answer these questions, the researchers developed one of the largest immune neoantigen atlases, evaluating 1,483 peptides. Eighty patients with non-small cell lung
cancer were enrolled in the study, and received the immunotherapy nivolumab.
Dr. Alban, data scientist Prerana Parthasarathy and their colleagues sampled the tumors prior to the patients initiating immunotherapy. They further sampled the same tumors once patients were on therapy to identify which antigens were reduced during treatment.
This time-consuming endeavor involved:
• Performing exome sequencing of the tumors
• Identifying mutations
• Using computational methods to predict which peptides would be recognized by the immune system
• Creating patient-specific peptides
• Matching each peptide to the right patient’s HLA type
• Testing patient’s T cells for their capacity to recognize the HLA/peptide pair
“This work is very complex and requires many man hours in the lab, along with a strong computational effort,” says Dr. Alban.
Advertisement
Previously, it was believed that patients who didn’t respond to immunotherapy had no immune response, but the study showed this was not the case. “One of the unexpected findings was that non-responders also have an immune response to different antigens. They’re just not the right antigens,” explains Dr. Alban. “They tend to be much lower in frequency, so the tumor doesn’t respond clinically.”
“If you have neoantigens and the body isn’t responding, there’s something else blocking the activity or the ability of the immune system to hit tumor cells,” says Dr. Chan. “The dream is to target those new processes to identify new avenues for drug development.”
After the discovery of neoantigens, one big question in the field was how many neoantigens were needed to destroy a tumor. The team demonstrated that to achieve a complete response, you need to attack the various types of cells in that tumor. That means the body needs not just a high volume of neoantigens, but it needs the right combination of neoantigens.
“That’s what the study gets to the heart of -- not how activated or inactivated the immune system is but how the immune system is actually recognizing and responding,” says Dr. Alban.
The researchers are collaborating with the IBM Discovery Accelerator group to perform more advanced modeling on the data sets they created to identify factors that contribute to the immune response to these peptides. “What we hope is that the data sets can be used for machine learning to develop new models that may be useful for vaccine development and immunotherapy response prediction,” says Dr. Alban.
Advertisement
Advertisement

Collaborative patient care, advanced imaging techniques support safer immunotherapy management

Highly personalized treatment shrinks tumors resistant to immunotherapy

Cleveland Clinic Cancer Institute among select group of centers to administer highly personalized treatment

Patients receive specialized inpatient and outpatient care for cellular, gene and immune cell-engaging therapies
Clinicians highlight the need to educate patients about warning signs

Immune toxicity remains a diagnosis of exclusion, and multidisciplinary collaboration remains the cornerstone for early diagnosis and treatment.

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies