Clinicians highlight the need to educate patients about warning signs
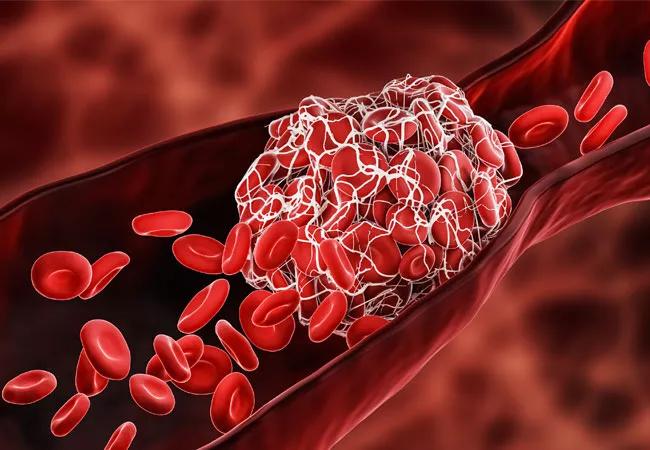
Although it has been known for some time that immunotherapies such as immune checkpoint inhibitors increase the risk of blood clots, clinicians – and many patients – may be surprised to hear how common these are. A Cleveland Clinic study demonstrated that for certain types of cancer, up to one in five patients taking immune checkpoint inhibitors are at risk of venous thromboembolism (VTE), arterial blood clots, stroke or myocardial infarction. These adverse events are even more likely to occur if the patient is receiving two types of immunotherapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Since the initial study, several research teams have validated these findings. In a follow-on study of 374 patients (mostly with lung cancer or melanoma) receiving immune checkpoint inhibitor therapy such as nivolumab, 13.4% of patients experienced VTE.
Since survival is vastly improved with the use of these therapies, patients are on these medications much longer than traditional treatments like chemotherapy. Because of this, the study authors noted that “rates of VTE should be considered by time interval because exposure time is more longer than with traditional treatments. The one-year cumulative incidence of VTE was also high, at 12.2%.”
The risk of VTE in patients receiving two immunotherapies was 29.3%. In addition, patients who developed other immune-related toxicities were more likely to experience VTE (17.4%). Notably, VTEs appear to have been under reported in early randomized trials of ICI therapy conducted prior to drug approval.
Although blood clots are very manageable with anticoagulants such as rivaroxaban or apixaban, patients often are not aware of the warning signs of these conditions. If a patient experiences sudden onset chest pain or shortness of breath, a cough with bloody sputum, unilateral leg swelling or sudden calf pain, they should seek urgent care. “That is not a situation where the patient should wait and see if it gets better,” says Alok Khorana, MD, Vice Chair to Director, Gastrointestinal Malignancies Program at Cleveland Clinic Cancer Center. “These are all very concerning warning signs of deep vein thrombosis or pulmonary embolisms, and we need to make patients aware of this.”
Advertisement
Often either by prevention or immediate treatment, a clot can be managed or prevented from occurring in the first place. “Anticoagulants are usually highly effective in controlling clots,” says Dr. Khorana. “Ideally, swift intervention will also avoid disruption to the patient’s cancer treatment.”
Beyond patient education, Dr. Khorana and his team are immersed in studies of why immune checkpoint inhibitor therapy often leads to blood clots. Building on their initial work, the team secured an NIH grant to better understand this phenomenon.
Their next step involves identifying potential candidate biomarkers to predict which patients will contract blood clots. At the same time, the team is enrolling 1,000 patients in a study to pinpoint precisely which molecules are leading to the increased risk of these clinical events.
“We don’t yet know what is causing clots to occur in these patients,” explains Dr. Khorana. “One aspect is that immunotherapy revs up the body’s immune system and in doing so, it creates an inflammatory state that is an environment that can lead to clots.”
The hope is that by better understanding risk factors and the underlying mechanisms of clots, researchers can reduce the risk and prevent many of these incidents from occurring.
Advertisement
Advertisement

Collaborative patient care, advanced imaging techniques support safer immunotherapy management

Highly personalized treatment shrinks tumors resistant to immunotherapy

Cleveland Clinic Cancer Institute among select group of centers to administer highly personalized treatment

Researchers develop first-of-its-kind neoantigen atlas to better understand immunotherapy resistance

Patients receive specialized inpatient and outpatient care for cellular, gene and immune cell-engaging therapies

Immune toxicity remains a diagnosis of exclusion, and multidisciplinary collaboration remains the cornerstone for early diagnosis and treatment.

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient