Researchers analyze pre and postoperative neuropsychological performance

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7e077e0c-484b-49c2-899b-eccbb3a1284f/22-CHP-3073158-CQD-Pediatric-Perspectives-Kauer-Busch-hero_jpg)
22-CHP-3073158 CQD- Pediatric Perspectives-Kauer-Busch-hero
By Navkiranjot Kaur, MD and Robyn Busch, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Surgical resection of the epileptogenic zone results in seizure freedom in up to 70% to 80% of children with pharmacoresistant epilepsy1; however, the cognitive risks of pediatric epilepsy surgery remain unclear. Compared to the more extensive adult literature, studies on the cognitive risks of pediatric epilepsy surgery are fewer and the results are inconsistent. Existing studies have been limited by small sample sizes, varying sample characteristics, group-level analyses, and/or non-empiric methodologies.
Reliable change indices (RCIs) are an empiric methodology in the field of neuropsychology used to assess clinically meaningful cognitive change over time or following an intervention. RCIs are more accurate than traditional methods (e.g., one standard deviation (SD) change) for assessing cognitive change as they control for factors that may impact postoperative test scores in the absence of any underlying change (e.g., imperfect test reliability, measurement error, practice effects). Thus, RCIs allow for an empirically-based determination of what constitutes a clinically meaningful change in cognition due to surgery rather than relying upon clinical judgment or an arbitrary cut-off value.
We designed a retrospective cohort study to characterize outcomes following pediatric epilepsy surgery across a broad range of cognitive domains using empirical RCI methodology, compare these outcomes with those based on traditional methods (i.e., SDs), and identify factors associated with postoperative cognitive declines and/or improvements.2
Advertisement
The study included 186 children, ages 6 to 16 years, who underwent resective brain surgery for treatment of pharmacoresistant epilepsy and who completed pre and postoperative neuropsychological assessments. All children completed measures of intelligence, attention/working memory, processing speed, language, executive functioning, visuospatial skills, memory, and academic achievement both before and after surgery.
Change scores from pre to postoperative assessments were classified as decline, no change, or improvement using published RCIs developed in children with epilepsy who did not undergo surgery (80% confidence interval).3 Chi-square goodness of fit tests compared the distribution of outcomes as defined with RCIs to those obtained using a traditional one standard deviation cutoff. Multinomial regression analyses were used to identify factors associated with cognitive decline and/or improvement.
Approximately 6.5 months following surgery, the overall rates of RCI decline ranged from 4% to 35%, and the rates of RCI improvement ranged from 2% to 31% on individual cognitive measures. Compared to RCIs, SD methodology often overestimated postoperative improvements and varied with respect to declines. Encouragingly, most children demonstrated relatively focal changes (declines and/or improvements in one to two domains) and very few demonstrated more global changes (declines and/or improvements in three or more domains).
Of the sample, 46% of the children did not demonstrate declines in any cognitive domain and over half the sample demonstrated cognitive improvement in at least one cognitive domain. When cognitive declines did occur, they were typically restricted to one or two cognitive domains (Table).
Advertisement
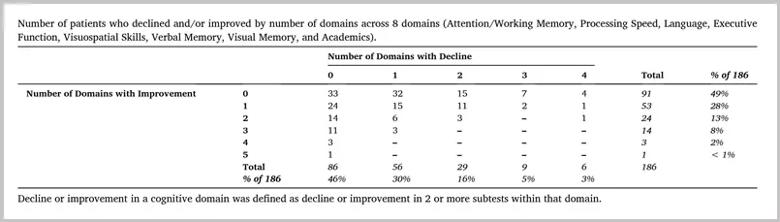
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/687e0f42-f578-44b3-8b1c-311e22cbb0a6/22-CHP-3073158-CQD-Pediatric-Perspectives-Kauer-Busch-v2-inset_jpg)
Table. Reprinted with permission from Elsevier. Kaur N, Nowacki AS, Haut JS, et al. Cognitive outcomes following pediatric epilepsy surgery. Epilepsy Res. 2022;180:106859. doi:10.1016/j.eplepsyres.2022.106859
Better preoperative cognitive performance was associated with higher odds of postoperative decline and lower odds of postoperative improvement across most cognitive domains. Age at the time of surgery, surgery site and postoperative seizures were also variably associated with postoperative change across several cognitive domains.
Our results suggest variability in individual, short-term cognitive outcomes following resective brain surgery for epilepsy in children. The differences in change distributions obtained using epilepsy-specific RCIs versus SDs highlight the need for studies using an empiric methodology to study postoperative cognitive change.
Although longer-term studies are certainly required, these short-term outcomes remain important as early identification of children at risk for cognitive decline allows for timely implementation of interventions such as cognitive rehabilitation. This study will serve as an important comparator for future longer-term studies of postoperative cognitive outcomes in children.
Future studies may build on this work by developing multivariable prediction models to identify individual children who are likely to demonstrate postoperative cognitive declines and/or improvements to aid clinical decision-making and patient counseling.
About the authors: Dr. Kaur studied cognitive outcomes following pediatric epilepsy surgery as a medical student at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University under the mentorship of Dr. Robyn Busch. She is now pursuing internal medicine residency training at the University of Michigan.
Advertisement
Dr. Busch is Head of the Section of Neuropsychology in the Center for General Neurology and a Staff Neuropsychologist in the Charles Shor Epilepsy Center within the Neurological Institute at Cleveland Clinic. She is also Associate Professor of Neurology in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
References
1. Dwivedi R, Ramanujam B, Chandra PS, et al. Surgery for Drug-Resistant Epilepsy in Children. N Engl J Med. 2017;377(17):1639-1647. doi:10.1056/nejmoa1615335
2. Kaur N, Nowacki AS, Haut JS, et al. Cognitive outcomes following pediatric epilepsy surgery. Epilepsy Res. 2022;180:106859. doi:10.1016/j.eplepsyres.2022.106859
3. Busch RM, Lineweaver TT, Ferguson L, Haut JS. Reliable change indices and standardized regression-based change score norms for evaluating neuropsychological change in children with epilepsy. Epilepsy Behav. 2015;47:45-54. doi:10.1016/j.yebeh.2015.04.052
Advertisement
Advertisement
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology
Recommendations on identifying and managing neurodevelopmental and related challenges
Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies
Aim is for use with clinician oversight to make screening safer and more efficient
Rapid innovation is shaping the deep brain stimulation landscape
Study shows short-term behavioral training can yield objective and subjective gains