Youth and open physes are two factors that increase risk of recurrence

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ef1f3547-ab52-4f49-837d-cf37625980cf/22-ORI-3198758-CQD-650x450-1_jpg)
22-ORI-3198758 CQD 650×450
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Patellar instability is quite common, with incidence estimated at 5.8 per 100,000 in the general population. In the 10- to 17-year-old age group, the incidence can be as high as 29 per 100,000. The rate of recurrence following a first-time patellar dislocation has been estimated at anywhere from 15% to 44%.
Historically, patients with first-time patellar dislocations have been treated without surgery due to expected low rates of recurrence and high rates of success with nonoperative treatment. However, more recent literature suggests that benign neglect may not be as benign as once thought, and recurrent dislocation may be very high in certain patient populations.
It is now known that patients treated conservatively may have significant disability following nonoperative management of patellofemoral dislocation. Straume-Næsheim et al showed that patients with recurrent lateral patella dislocation had more pain and dysfunction and worse quality-of-life scores than patients with anterior cruciate ligament-deficient knees.
Several factors have been associated with poor pain and function following patellar instability. We recently showed that higher body mass index, female sex, older age and lower mental health scores were associated with higher pain scores in patients with patellofemoral instability.
Some of the disability in patients treated conservatively following first-time patellofemoral instability may be related to the presence of recurrent dislocation and/or subluxation. While the risk of recurrent dislocation following an index patellar dislocation is low (approximately 33%), the risk is much higher in some patients.
Advertisement
In a systematic review by Huntington et al, the risk of recurrent dislocation was higher in patients who are younger and/or have:
Of these factors, trochlear dysplasia was found to be the most important factor implicated in patellofemoral instability, with an odds ratio of 4.15. When no risk factors were found, the risk of dislocation was 7.7% to 13.8%. When two risk factors were present, the risk increased to 29.2% to 60.2%. The risk of re-dislocation with three risk factors was 70% to 78%.
Determining the risk of recurrent dislocation is important to help patients and families make the best decision about further management. Explaining to an older patient with no radiographic risk factors that the risk of re-dislocation is less than 13% often impacts differently than telling a skeletally immature patient with additional risk factors that the risk of recurrent instability is greater than 80%. The latter may be more inclined to consider surgical intervention.
In order to determine recurrent dislocation risk and best counsel patients, we have more recently become proponents of obtaining MRI at the time of the index patellar dislocation. Along with plain films that are performed on every patient, MRI is used to assess key risk factors.
We generally use plain X-ray to evaluate patellar height and trochlear dysplasia. We use the Caton-Deschamps index to evaluate for patella alta (Figure 1). A value above 1.2 is considered abnormal. Trochlear dysplasia is best seen on a perfect lateral X-ray and graded using Dejour classification (Figures 2 and 3).
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3a460643-d8af-4502-85cf-5b3529667ed2/22-ORI-3198758-inset-1_jpg)
Figure 1. Caton-Deschamps index. The distance from the inferior articular surface to the anterosuperior corner of the tibia (B) is measured by length of the patellar articular surface (A).
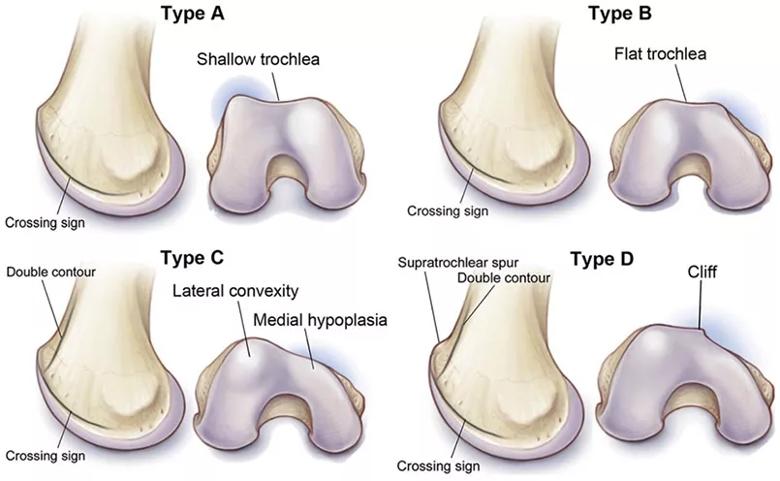
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5f9ec9bf-cf96-48b1-80ad-a7d71c9def52/22-ORI-3198758-inset-2_jpg)
Figure 2. Illustration of the Dejour classification system.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e13cba5b-e37a-4f0f-9c04-53f01646279a/22-ORI-3198758-inset-3_jpg)
Figure 3. Radiographic examples of the Dejour classification. Dejour Type A trochlea (A), Dejour Type B trochlea (B), Dejour Type C trochlea (C), Dejour Type D trochlea (D).
Trochlear dysplasia is not uncommon. In a recent epidemiologic study, we showed that trochlear dysplasia was present in 39% of knees. However, moderate to severe dysplasia was present in only 17%.
MRI is the modality of choice to determine TT-TG distance. TT-TG values greater than 20 mm are considered abnormal. Patellar height also can be determined on MRI by using the patellotrochlear index (PTI). When less than 18%, the PTI is considered abnormal.
Even without abnormal indices on imaging, our skeletally immature patient population is at an increased risk of recurrent dislocation as they, by definition, present with two risk factors: age and open physes. With the addition of one or two other risk factors, these patients have a greater than 80% chance of recurrence.
Knowing the increased pain, disability and lower quality-of-life scores that are caused by symptomatic patellofemoral instability, it is reasonable to consider early surgery for young patients at high risk of recurrent dislocation rather than pursuing conservative management. Patellofemoral stabilization surgery, including medial patellofemoral ligament reconstruction, is extremely successful, with high rates of patient satisfaction and improved function.
Advertisement
Dr. Farrow is an orthopaedic surgeon at Cleveland Clinic Sports Medicine Center. He also serves as Director of Clinical Operations for Sports Medicine.
Advertisement
Advertisement
Computer simulation identifies causes of instability
How it’s similar but different from the direct anterior approach
Collaboration must cross borders and disciplines
Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols
Should surgeons forgo posterior and lateral approaches?
How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians
Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes
Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction