Pars plana vitrectomy can provide long-term control of intraocular pressure
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
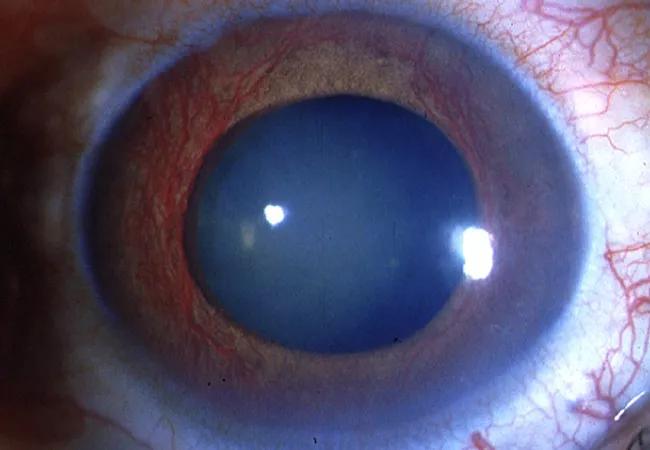
A 66-year-old man with known proliferative diabetes presented with acute left eye pain. His intraocular pressure (IOP) was 25 in the right eye and 48 in the left eye. He had been using dorzolamide/timolol and brimonidine eye drops, but had run out of them one month prior. Upon examination, the patient had an inferior hyphema in his left eye with microcystic edema, 20/100 visual acuity and a vitreous hemorrhage. In the right eye, he had neovascularization of the iris with cupping of the optic nerve and obvious neovascularization elsewhere.
Neovascular glaucoma cases like this are challenging and require a coordinated approach by glaucoma and retina specialists. Unfortunately, a standardized care path has not been established by the ophthalmology community. A 2019 Cleveland Clinic study showed that while many glaucoma and retina specialists agree on using anti-VEGF medication as a first-line treatment, they do not concur on subsequent steps, particularly surgical approach.
Cleveland Clinic’s Cole Eye Institute has developed its own protocol for managing patients with neovascular glaucoma. I outlined this care path, which involves both glaucoma and retina specialists, during glaucoma subspecialty day at the American Academy of Ophthalmology (AAO) 2020 virtual meeting.
Retina specialists at Cole Eye Institute are involved in the care of patients with neovascular glaucoma at three points:
Advertisement
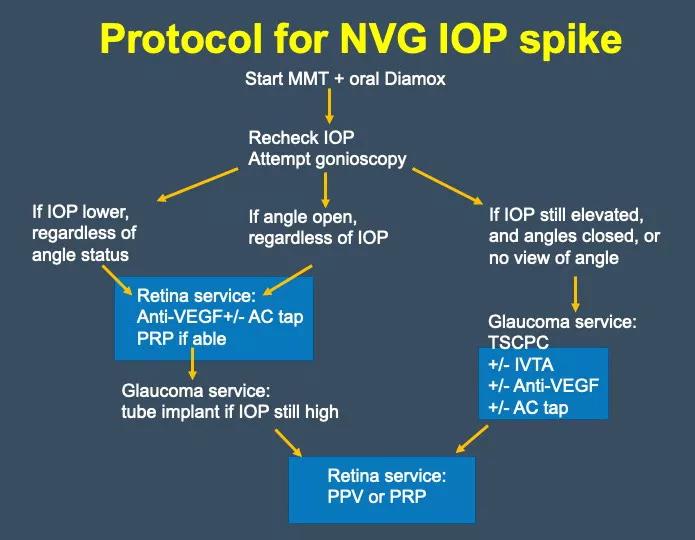
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/68e1aede-d7c8-492e-aca7-0e7f53dd3ed4/20-EYE-2010962-Neovascular-Glaucoma-CQD-Inset_jpg)
Cole Eye Institute’s protocol for treating neovascular glaucoma involves both glaucoma and retina specialists.
Retina service is highlighted in blue.
TSCPC can reduce aqueous production when outflow is restricted. It’s very effective at treating refractory neovascular glaucoma. In fact, it is comparable to valve implants at lowering IOP over six months.
At Cole Eye Institute, retina specialists give preoperative anti-VEGF therapy to patients undergoing TSCPC and give concurrent intravitreal triamcinolone acetonide as we’ve found that it reduces risk of eye pain, iritis, corneal edema, cystoid macular edema, hypotony and phthisis. We also perform pars plana vitrectomy — placing tubes in the posterior segment — when needed. This usually happens in patients who have a compromised cornea, inadequate space in the anterior chamber, scarred conjunctival tissue or concurrent vitreoretinal disease.
Typically, the glaucoma team will first address the conjunctiva, place the plate of the tube implant if needed or extract an existing tube from the anterior chamber. Then a retina team will perform the vitrectomy, creating a depression in the area the tube will be implanted by shaving the vitreous base. A sclerotomy also can be used by the glaucoma team to implant the tube, if it’s well aligned.
Recent advances, such as the Pars Plana Clip™ and Hoffman elbow, allow for complete perpendicular implantation of tubes within the vitreous cavity.
There are certainly complications to posterior tube implantation: vitreous hemorrhage, vitreous incarceration, retinal detachment, kinking or displacement of the tube, and choroidal effusion or hemorrhage if the tube is placed incorrectly. If the tube runs through the visual axis it also can cause a decrease in visual acuity.
Advertisement
However, long-term outcomes in patients with posterior tube implant are comparable to those of patients with anterior tube implant. In a 2018 study of patients at Cole Eye Institute, 57 with pars plana vitrectomy and 57 with an anterior chamber tube, we found equivalent declines in IOP following surgery in both groups over 60 months. This is the longest-term study of pars plana tubes currently available. Our overall success rate — defined as IOP of 6-21 mm/Hg (on or off medications), no loss of light perception vision and no need for another glaucoma surgery — was 86% with the pars plana tube and 80% with the anterior chamber tube.
There were some postoperative complications, including diplopia, hypotony, vitreous hemorrhage, tube erosion and corneal decompensation. But these complications occurred in both groups.
In summary, pars plana glaucoma drainage implants can provide long-term IOP control with a low risk of tube exposure. A partnership of glaucoma and retinal specialists can be beneficial for patients with neovascular glaucoma as well as patients who have had multiple failed anterior chamber tubes.
Dr. Singh is a staff surgeon at Cleveland Clinic’s Cole Eye Institute. He specializes in retinal disease, including diabetic retinopathy and age-related macular degeneration.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift