Advertisement
Results from 15 years of follow-up in over 500 neonates

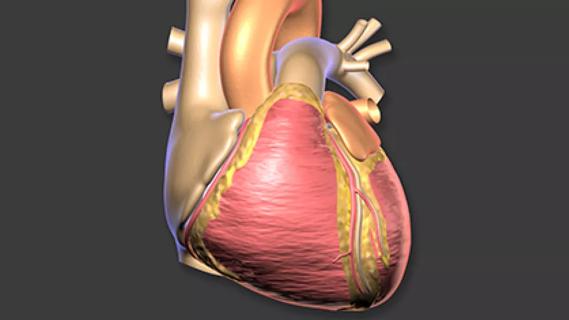
Follow-up of a large cohort of neonates with aortic valve atresia through adolescence reveals that long-term survival is greater with primary heart transplantation than with surgical palliation. Use of transplant as a rescue strategy for failed surgical palliation is not as favorable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
These are lead findings in a new report from a multi-institutional study of the Congenital Heart Surgeons’ Society (CHSS) database published in the Journal of Thoracic and Cardiovascular Surgery. The study is the first of its kind to describe how survival through adolescence varies according to initial treatment strategy in this patient population.
“We didn’t know what to expect about survival of neonatal transplant patients, so this was new information for us, but not necessarily a surprise,” says study co-author Eugene Blackstone, MD, Head of Clinical Investigations in Cleveland Clinic’s Heart, Vascular & Thoracic Institute.
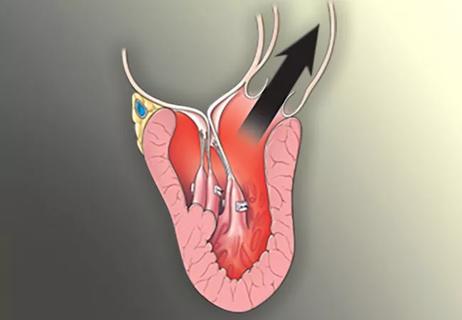
From 1994 to 2000, 565 neonates with aortic atresia were admitted to 26 North American hospitals participating in the CHSS database, including Cleveland Clinic. Within 10 days of birth, the vast majority underwent surgical palliation (n = 453) or listing for primary cardiac transplantation (n = 68). Six patients underwent biventricular repair, and 38 received supportive care only.
At 15 years of follow-up, survival was greater with primary transplantation (including wait list mortality) than with surgical palliation (65% vs. 40%; P = 0.002), although survival was reduced in patients receiving secondary transplantation (48% at 9 years).
The study was designed to also assess the treatments’ relative impact on patients’ quality of life over time. In this regard, self-reported quality of life (as measured with the PedsQL™ instrument) was similar in the surgical palliation and transplant groups, although patients who underwent transplantation experienced significantly fewer symptoms as adolescents.
“We expected the adolescents who had heart transplants to have a better quality of life than those who were surgically palliated, but both groups reported a quality of life lower than that of healthy peers and comparable to that of adolescents with chronic diseases,” says Dr. Blackstone, one of the co-founders of the CHSS database.
“These children face a lot of challenges — physically, emotionally and developmentally,” adds study co-author Gosta Pettersson, MD, PhD, Vice Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic. “They have a limited quality of life and are bound to medical institutions and doctors. It’s a hard road for them and their families.”
The study cohort underwent treatment in an era (1994 to 2000) when management strategies to stabilize neonates presenting with hypoplastic left heart physiology were evolving. This led some reviewers to critique the study group as “old.”
“Unfortunately, if you want to know what happens after 15 years, you have to wait 15 years to find out,” Dr. Pettersson quips.
Since 2000, survival after surgical palliation — particularly with the Norwood procedure — has greatly improved.
Advertisement
“Here at Cleveland Clinic, we have not had a Norwood mortality in the past four years,” notes Hani Najm, MD, Chair of Pediatric and Congenital Heart Surgery at Cleveland Clinic. “For two consecutive years now, our mortality rate for all surgeries for congenital heart disease has been less than 1%.”
He attributes the improved outcomes to multiple factors, including better surgical, anesthetic and perfusion techniques; increased understanding of patients’ postoperative and ICU courses; and early-warning monitors that enable physicians to intervene if problems get out of hand.
Does this mean surgical palliation might produce better outcomes than transplantation today?
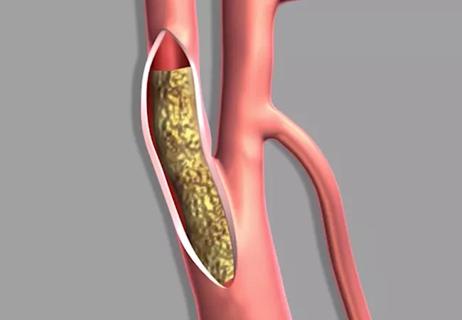
It’s unlikely, says Dr. Blackstone. “The serious problems of a heart with a single pumping chamber after the Fontan operation remain unsolved,” he explains. “Even in contemporary practice, unless there are breakthroughs in managing patients with surgical palliation, lifespan will be shorter than in the general population. This reflects the palliative nature of this strategy. Hopefully the problems of living on a single ventricle can be improved. But without a breakthrough, the natural history of surgical palliation remains as we predicted it would be 30 years ago.”
For unknown reasons, heart transplantation in newborns produces better long-term outcomes than transplants performed later in life.
“The chances of survival with good functioning are better than with palliation,” says Dr. Pettersson. “If we had an unlimited supply of hearts, transplantation would almost always be preferable. However, the likelihood of obtaining a neonatal donor heart within a reasonable amount of time remains poor.”
The option to transplant also raises important issues related to allocation of a scarce resource. After all, surgical palliation is not an option for some other critical congenital heart defects. “We must be judicious with the few hearts we have,” Dr. Pettersson notes.
With improved and much lower early mortality with the Norwood procedure, as well as a typical waiting time of at least six months for a newborn heart, Cleveland Clinic offers surgical palliation over transplantation for most patients.
“In the case of a late failure, transplantation is still an option,” Dr. Najm observes.
Primary transplantation also may be considered for neonates with risk factors predictive of exceptionally poor survival after surgical palliation — e.g., presence of anomalous coronary arteries, endocardial fibroelastosis, a restrictive atrial septum or other organ-associated anomalies.
Advertisement
“The key message from this study is to keep primary transplantation as an option for complex anatomy and predicted poor outcome from palliation with the Norwood procedure,” Dr. Najm says.
“Whether a patient undergoes transplant or surgical palliation, lifelong surveillance is essential,” adds Dr. Blackstone. “These adolescents need to be transitioned deliberately to the care of either a transplant cardiologist or a cardiologist well versed in problems of the palliated Fontan patient.”
Advertisement
Advertisement

Surprise findings argue for caution about testosterone use in men at risk for fracture

Findings support emphasis on markers of frailty related to, but not dependent on, age
![GettyImages-1252287413 [Converted]](https://assets.clevelandclinic.org/transform/StoryPanel/350804b2-f1e4-4d97-a277-9629cf45af3e/23-HVI-4120348_redlining_650x450_jpg?w=3840&q=75)
Large database study reveals lingering health consequences of decades-old discrimination
Additional analyses of the two trials presented at 2023 ESC Congress
Prospective SPIRIT-HCM trial demonstrates broad gains over 12-month follow-up

An ACC committee issues recommendations to accelerate sluggish progress
Review of our recent experience shows it’s still a safe option
Machine learning may improve risk prediction and guide therapy