Growing awareness of impact leads to proliferation of procedures
Anomalous aortic origin of a coronary artery (AAOCA) is an important cause of sudden cardiac arrest, most notoriously occurring in young athletes with no inkling of underlying problems. But awareness is increasing that this rare congenital malformation with multiple variants can also cause trouble in adults, as can myocardial bridges, a more common defect involving part of a coronary artery course embedded within the myocardium.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Because most cardiologists and surgeons typically see few adults with AAOCA, or have the misconception that all myocardial bridges are benign, there is much uncertainty about what is benign or malignant and what intervention, if any, is needed,” says cardiologist Joanna Ghobrial, MD, MS, Medical and Interventional Director of Cleveland Clinic’s Adult Congenital Heart Disease Center. “Having gained more experience with these patients in recent years, we can recommend some optimal strategies for evaluation and management.”
Cleveland Clinic has become one of the highest-volume centers in the country for handling these unusual and complex anomalies in adults. Over the past two decades, Cleveland Clinic clinicians have developed novel approaches — using noninvasive and invasive evaluation as well as surgical techniques — to address them.
AAOCA and myocardial bridges can cause ischemia due to compression or kinking of the coronary artery. As a result, patients may present with fatigue, dizziness or fainting, shortness of breath, atypical chest pain or anginal symptoms. Since such symptoms can also arise from coronary atherosclerosis or aortic valve disease, teasing out the cause can be complicated in adults with cardiovascular comorbidities.
However, some patients may be asymptomatic, with AAOCA and/or myocardial bridges discovered incidentally, sometimes by CT evaluation after an injury or during workup for other causes. While AAOCA in adulthood was once thought to be not as malignant as AAOCA discovered in youth, this is now known to be inaccurate and it is recognized that the first symptomatic manifestation may be cardiac arrest, which means that an incidental finding should be taken seriously. And although many myocardial bridges may indeed be benign, a portion of them can cause limiting symptoms and lead to myocardial infarction and malignant arrhythmias as well as cardiac arrest.
Advertisement
“Anyone who is discovered to have AAOCA, whether incidentally or during a workup for atypical symptoms, should have a thorough evaluation,” says Dr. Ghobrial. “On the other hand, given that myocardial bridges are more common, patients who are asymptomatic may not require further investigation, while those presenting with concerning symptoms with no other clear etiology should undergo an investigative protocol like the one we employ.”
To assess whether an intervention is indicated, Cleveland Clinic surgeons and cardiologists conduct a variety of tests, including:
Once the situation is thoroughly understood, the clinical team collaborates with the patient and family to determine next steps. The potential benefit of intervention is balanced against operative risk.
“Our approach is one of shared decision-making with our patients, integrating their desires for active lifestyles,” says Tara Karamlou, MD, MSc, Surgical Director of the Adult Congenital Heart Disease Center. “We may treat a professional athlete more aggressively than an older patient who may not desire to be as physically active. That said, we have operated on patients as old as 75, including physically active grandparents who wanted reassurance that they wouldn’t be limited caring for their grandchildren.”
Advertisement
Although Cleveland Clinic surgeons frequently see patients with AAOCA or myocardial bridges who were treated elsewhere with CABG and stents, they do not recommend this strategy unless the patient has concomitant coronary artery disease in the involved vessel.
“Bypass grafts are more at risk for competitive flow in AAOCA cases, and coronary stents may also be problematic in these situations,” Dr. Karamlou notes. “Dynamic compression in these anomalous arteries and the competitive flow may lead to poor perfusion, making the graft or stent prone to failure and complicating further intervention.”
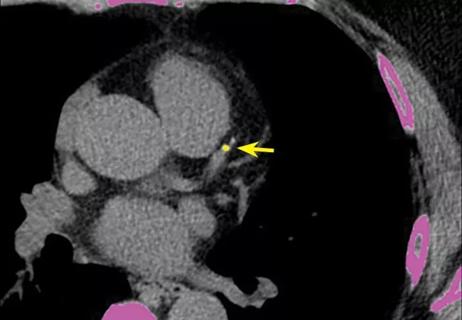
Instead, she recommends unroofing and rerouting procedures (see below), with approaches tailored to the specific anomaly. Postoperatively, intravascular ultrasound and cardiac catheterization with dobutamine stress testing is repeated to determine normalization of blood flow to the myocardium.
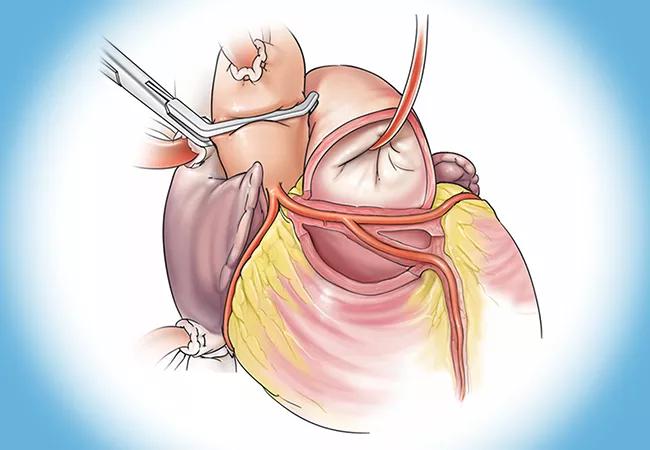
Electrocautery for unroofing. Over the years, the unroofing approach at Cleveland Clinic has changed from traditional sharp excision to electrical fulguration of the shared intramural wall segment (Figure 1). This method, which was developed by Cleveland Clinic surgeons, has been shown to be equally safe and effective with shorter cardiopulmonary bypass and cross-clamp times (Ann Thorac Surg. 2019;107:P823-P828).
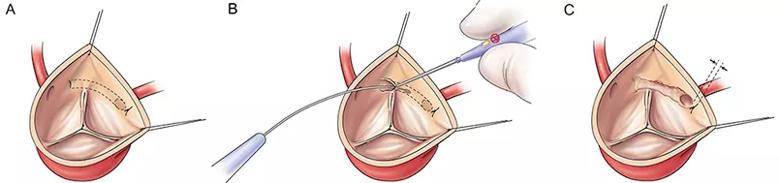
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7c83a7d5-85dd-4022-bb48-ddcd324b8a03/22-HVI-3413074-CQD_Inset-1_jpg)
Figure 1. Illustration of key steps in the Cleveland Clinic-developed electrical fulguration technique for coronary unroofing for AAOCA. Reprinted with permission from Vinnakota et al., Annals of Thoracic Surgery(2019;107:P823-P828), © 2019 by The Society of Thoracic Surgeons.
Advertisement
Vouhé technique.For an anomalous left coronary artery arising from the right sinus with an intramural course between the pulmonary artery and aorta, the more difficult Vouhé technique is required. This involves suturing a fresh autologous pericardial patch to create a new coronary ostium in the appropriate left sinus.
Najm procedure for transseptal anomalies.Hani Najm, MD, Chair of Pediatric and Adult Congenital Heart Surgery at Cleveland Clinic, developed the first operation to address a rare AAOCA of the left coronary artery with a transseptal course behind the right ventricular outflow tract. The procedure involves complete unroofing of the anomalous coronary artery within the ventricular septum and bridging it with pericardium (Figure 2). It was described in detail in 2019 (Ann Thorac Surg. 2019;108:e383-e386) and recently updated with midterm outcomes from 14 patients (Ann Thorac Surg. 2023;115:e29-e31).
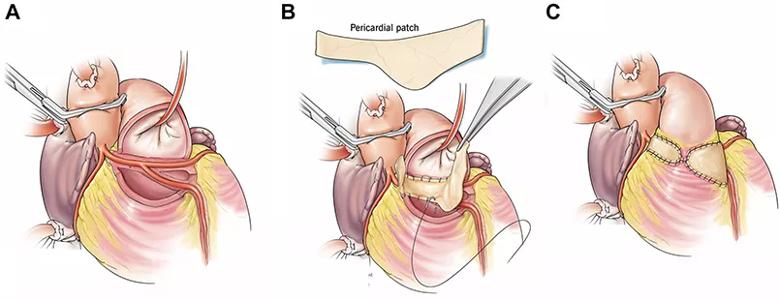
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1a21fa8f-46f7-4625-b385-e58cd3fb8f1b/22-HVI-3413074-CQD_Inset-2_jpg)
Figure 2. Illustration of key steps in the Najm procedure. (A) Anomalous aortic origin of the left coronary artery with a transseptal course and early takeoff of the left anterior descending artery (LAD) from the left main coronary artery. (B) Modified autologous pericardial patch shape to accommodate the high takeoff of the LAD. The patch is straight on the superior aspect and wider inferiorly. (C) Completed repair with closure of the anterior right ventricular outflow tract with autologous pericardium. Reprinted with permission from Najm et al., Annals of Thoracic Surgery (2023;115:e29-e31), © 2022 by The Society of Thoracic Surgeons.
Advertisement
“Currently, with 18 Najm surgeries completed at Cleveland Clinic, there have been no deaths,” says Dr. Najm. “Patients report resolution of symptoms, and postoperative testing indicates normalized perfusion.”
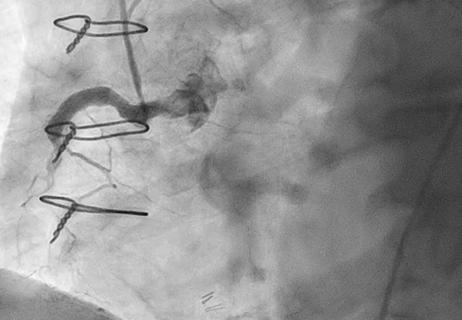
Myocardial bridge unroofing.“While myocardial bridges are often a benign incidental finding, deep and long ones tend to be more dangerous,” says cardiothoracic surgeon Shinya Unai, MD. “When the myocardium squeezes the embedded coronary artery with exercise, ischemia results.”
To surgically address this, Dr. Unai painstakingly removes the myocardial fibers above the coronary artery (Figure 3). He reiterates that a myocardial bridge should not be treated with a distal bypass, as the graft will only receive blood flow intermittently and will soon fail.
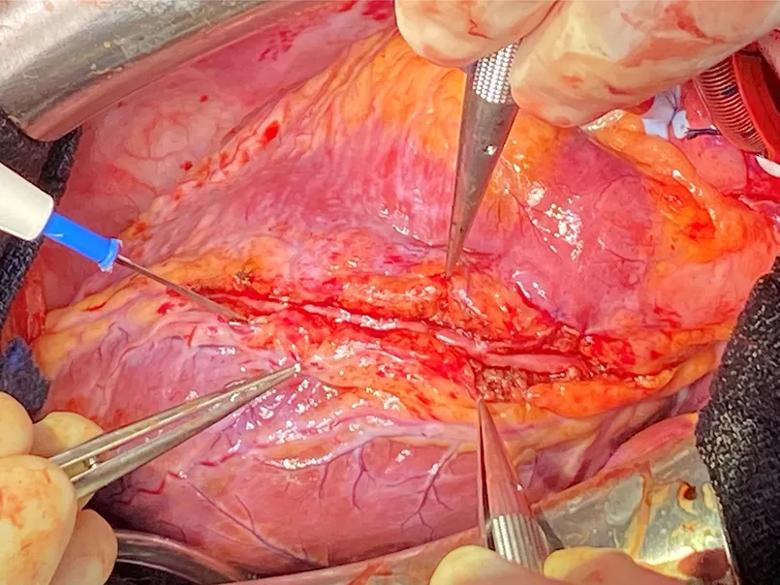
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c74dc5a6-da89-474e-92c2-be1b87a11b8e/22-HVI-3413074-CQD_Inset-3_jpg)
Figure 3. Photo after completion of bridge unroofing of the left anterior descending artery.
Cleveland Clinic is a member of the Congenital Heart Surgeons’ Society AAOCA registry, a network of institutions that pools data on patients diagnosed with AAOCA up to age 30 years. To address the shortage of data on older adults, Cleveland Clinic has developed a unique long-term database and registry to follow adults with AAOCA over time. These databases are enabling characterization of the multiple variants of AAOCA and outcomes of various surgical treatment strategies, including analysis of outcomes based on baseline imaging evaluation, noninvasive and invasive stress testing, and referral for surgery.
A review of 167 adults presenting with AAOCA during a two-year period at Cleveland Clinic was published in the Annals of Thoracic Surgery (2021;112[4]:1299-1305). Most patients presented with chest pain or shortness of breath. Right coronary artery anomalies were most common (57%), in contrast to the situation in pediatric patients. “This is probably a ‘lethal bias,’ in that left coronary artery anomalies are likelier to be fatal or addressed in childhood,” Dr. Karamlou observes.
Another study (JTCVS Open. 2022;10:205-221) characterized 763 patients with AAOCA from Cleveland Clinic databases and found no significant difference in the extent of coronary artery disease in anomalous coronary arteries versus normal arteries in the same individual.
Cleveland Clinic is also conducting novel research on the evaluative use of invasive dobutamine-stress testing and the potential role of noninvasive fluid-structure interaction modeling (JTCVS Tech. 2022;13:144-162). Such techniques may one day inform the need for surgery in AAOCA and myocardial bridge settings, as well as evaluate successful reperfusion postoperatively.
“We are currently looking into impacts of concomitant cardiac pathology, such as coronary artery disease,” Dr. Ghobrial notes. “Often such comorbidities make AAOCA patients develop symptoms after a lifetime of being asymptomatic, and they may complicate approaches to repair.”
Advertisement

5 biggest changes according to Cleveland Clinic experts
While procedural success rates lag overall, they shine for retrograde crossing
Lower success rates, more hospital MACE seen with poor-quality distal targets

Important additions to a novel surgical technique
Retrospective findings from an executive health program spur interest in broader studies

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve

Reproducible technique uses native recipient tissue, avoiding risks of complex baffles