Insights from guidelines and the Cleveland Clinic experience
Options for surgical treatment of infective endocarditis (IE) include valve repair, reconstruction or replacement. Guidelines generally recommend repairing the infected valve whenever possible. However, valve replacement is more commonly performed.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic researchers recently analyzed the outcomes of 2,760 aortic, mitral and tricuspid valve surgeries for IE performed at their institution from 2002 to 2022. In a presentation at the Society of Thoracic Surgeons annual meeting earlier this year, Shinya Unai, MD, Surgical Director of Cleveland Clinic’s Endocarditis Center, used the data to illustrate when infected valves should be repaired, which strategies to use for complex repairs and when replacement is the better option.
2016 consensus guidelines from the American Association for Thoracic Surgery (AATS) on the surgical treatment of IE say repair of native aortic valve IE may occasionally be possible when infection is limited to the valve cusps.
Of the 40 native aortic valve surgeries for IE performed at Cleveland Clinic in 2021, 39 were replacements or reconstructions. “There are not many situations where the aortic valve can be repaired — perhaps a single perforation in otherwise healthy-looking cusps,” Dr. Unai observes (see Figure 1).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c3561547-19f8-49f2-8fea-dd6172e19697/23-HVI-3655708-CQD-Inset1-1024x425_jpg)
Figure 1. For IE involving the aortic valve, repair is generally limited to cases such as a single perforation in otherwise healthy cusps (photo on left), whereas replacement is needed when multiple cusps are infected (photo on right).
When replacement is needed, reconstruction of the valve using the Ozaki procedure is an alternative to replacement with a prosthesis when the infection is limited to the cusps.
In the Ozaki procedure, the diseased valves are excised and replaced with cusps cut to size from autologous pericardium. The technique has multiple advantages, including no need for postoperative anticoagulation and superior hemodynamics.
Advertisement
An allograft may be beneficial when root reconstruction and replacement is needed, Dr. Unai notes. “We advise using an allograft for invasive aortic valve endocarditis with annular invasion,” he says, “as it is more flexible than a prosthetic valve, which makes it easier to place.”
He adds that the Ross procedure is another technique that can be performed to replace the aortic valve and reconstruct the aortic root for invasive disease. In this procedure, the aortic valve is removed and replaced with the patient’s pulmonic valve. The pulmonic valve is then replaced with a pulmonary allograft.
“The Ross procedure has long-term durability, making it particularly suitable for younger patients,” he explains. “The allograft has the ability to grow, and anticoagulation is not needed. Reinfection risk is the lowest among all strategies.”
Valve function is generally visualized with transesophageal echocardiography (TEE), but TEE is unable to reveal infection behind calcium deposits. “Aortic valve endocarditis can be complex, even if it doesn’t show on TEE or CT scan,” Dr. Unai says. “Surgeons need to be prepared to do a root replacement or place a homograft, if required.”
Sixty to 100 root replacements are performed at Cleveland Clinic every year, with a low 30-day mortality rate of 2% to 4%. “It is a technically demanding procedure, but fairly safe,” Dr. Unai observes.
According to the 2016 AATS guidelines, repair is the preferred option for mitral valve IE.
In a recent study (J Thorac Cardiovasc Surg. 2022 Apr 5 Epub), Dr. Unai and colleagues reviewed all isolated mitral valve surgeries performed at Cleveland Clinic between 2002 and 2020 to identify the factors that influenced outcomes. Of the 326 cases of native mitral valve infection, 120 were repairs and 200 were replacements.
Advertisement
“Patients needing standard repairs, such as for windsock lesions (Figure 2), did well,” he notes. “After more complex repairs, defined as lesions larger than 1 cm requiring large patches and NeoChords®, patients had higher rates of reoperation and mortality. Valve pathology requiring complex repairs is a surrogate of advanced disease, and a complex repair may not necessarily improve long-term outcome. In a sick patient, a replacement with a shorter cardiopulmonary bypass time may have a benefit.”
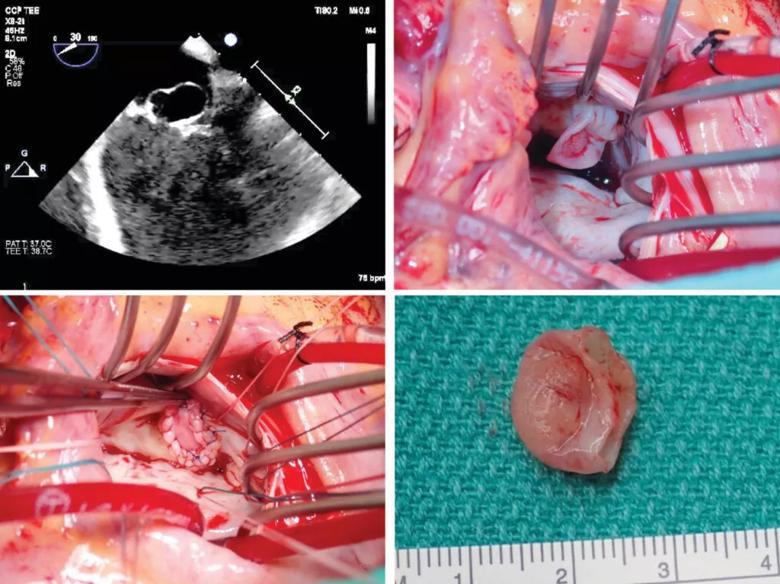
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/80789144-1df6-43f2-9cbf-0dde7e821b0a/23-HVI-3655708-CQD-Inset2-1024x767_jpg)
Figure 2. Echocardiogram and operative photos from a case of mitral valve IE requiring straightforward repair of a windsock lesion.
Extensive bileaflet infection should prompt replacement of the mitral valve, he says.
In the Cleveland Clinic experience, risk-adjusted outcomes of repair and replacement for mitral valve IE, including survival, have been similar in all groups.
“The message is simple,” says Dr. Unai. “Repair if it’s straightforward; if not, replace.”
The 2016 AATS guidelines recommend that repair of infected tricuspid valves be attempted whenever possible. Cleveland Clinic experience correlates with this recommendation. Of the 23 tricuspid valve IE cases seen in 2021, about 80% were repaired by resecting the infected and damaged tissue, patching the defect with pericardial tissue and adding NeoChords and an artificial ring.
Replacement is recommended when the entire valve is infected.
“We try very hard to repair, but if it doesn’t look like the valve can be repaired with less than moderate tricuspid regurgitation, I would replace it,” Dr. Unai advises.
Advertisement
Due to the proximity of the aortic valve to the mitral and tricuspid valves, IE infection can easily spread from the aortic valve to an adjacent valve.
Kissing lesions (Figure 3), in which floppy vegetations on the aortic valve touch the mitral valve, transferring the infection, are fairly easy to repair, says Dr. Unai.
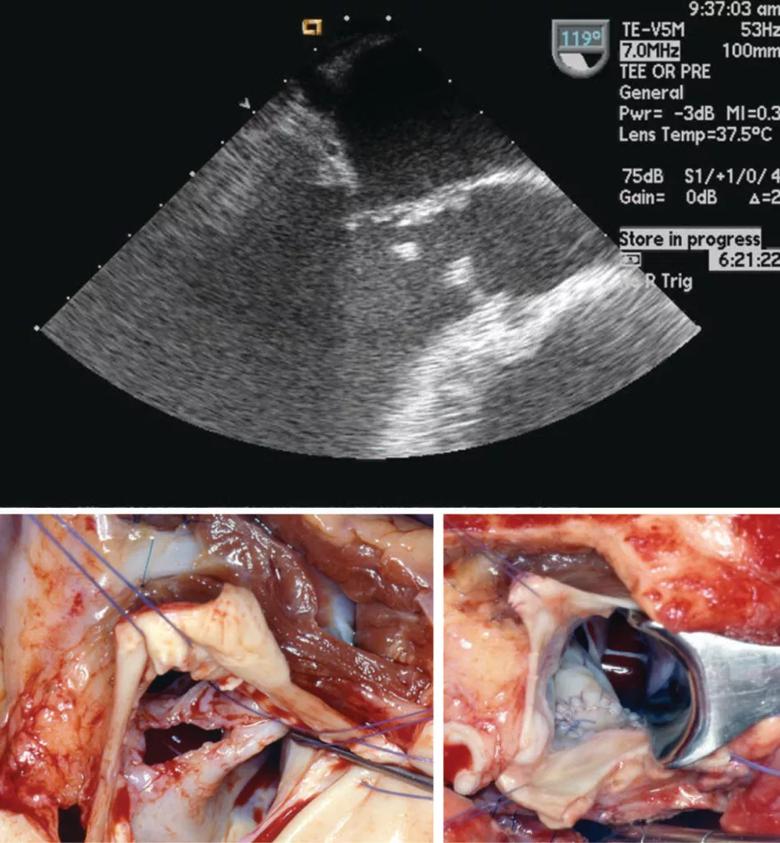
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/232331af-684c-4d7d-930e-15a76e339207/23-HVI-3655708-CQD-Inset3-947x1024_jpg)
Figure 3. Echocardiogram and operative photos showing a kissing lesion — in which IE vegetations spread from aortic to mitral valve — and its surgical repair.
Due to the proximity of the aortic valve to the mitral and tricuspid valves, IE infection can easily spread from the aortic valve to an adjacent valve.
Kissing lesions (Figure 3), in which floppy vegetations on the aortic valve touch the mitral valve, transferring the infection, are fairly easy to repair, says Dr. Unai.
It is incumbent upon surgeons who do not treat infected valves on a regular basis to learn these conditions and options. According to Dr. Unai, the overarching advice may be summarized in the following key points:
Moreover, surgical success depends on a solid foundation of comprehensive IE care. “Treating endocarditis effectively is a team sport in which each team member brings experience and expertise to diagnosis and management,” says Brian Griffin, MD, Section Head of Cardiovascular Imaging and an IE expert. “We are fortunate at Cleveland Clinic to have an Endocarditis Center with a highly experienced team comprising infectious disease physicians, imaging and valve disease physicians, and superb experienced surgeons. We often now use multimodality imaging, especially in complex endocarditis, including not just TEE but also CT and MRI and even PET scanning in specific situations. Our ability to recognize complex issues early, and therefore operate earlier than in the past, has led to substantial improvements in patient outcomes.”
Advertisement
“Approximately 50% of patients with infective endocarditis will require surgery either at diagnosis or as a result of valvular dysfunction after completing antimicrobial treatment,” adds Steven Gordon, MD, Chair of the Department of Infectious Disease. “Our Endocarditis Center brings together a multidisciplinary team to diagnose patients and offer treatment, which often combines surgery and antimicrobial therapy. When patients go to surgery, we review the histopathology with the cardiac pathology to confirm the diagnosis and extent of infection, and we use molecular methods (16S rDNA gene sequencing) to help determine the specific pathogen for most cases.”
Advertisement

Experts encourage customized care, concomitant treatment of substance use disorder and heart infection

Cleveland Clinic study points to need for new strategies to curb addiction relapse

Optimal management requires an experienced center

A closer look at the impact on procedures and patient outcomes

Join us in Florida this winter for a long-standing CME favorite

A scannable graphic recap of our latest data

International experts provide a guide for rapid decision-making focused on transcatheter options

TRISCEND II trial reports 1-year results